|




|
synonyms: Bankart repair, anterior instability repair
Arthroscopic Anterior Instability Repair CPT
Applicable ICD-10 Codes
- S43.004A-Unspecified dislocation of right shoulder joint, initial encounter
- S43.005A-Unspecified dislocation of left shoulder joint, initial encounter
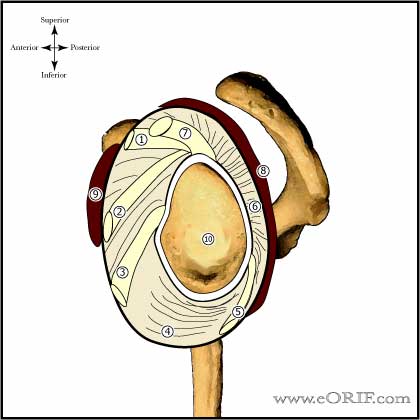
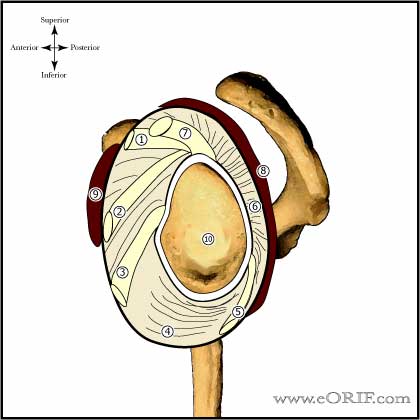
Arthroscopic Anterior Instability Repair Anatomy
- Anterosuperior plication affects external rotation of the adducted arm, decreasing it 30.1°. Anteroinferior plication reduces abduction by 19.4° and external rotation by 20.6°. Posterosuperior plication limits internal rotation of the adducted arm by 16.1°. Total anterior or total posterior plication limits flexion by 20° and abduction by 15° Total anterior plication limits external rotation by >30°.Total posterior plication limits internal rotation by >20°. Total inferior plication limits abduction by 27.7°, and also limits flexion, and rotation. Total superior plication restricts external rotation and flexion. (Gerber C,JBJS 2003A;85:48).
Arthroscopic Anterior Instability Repair Indications
- Recurrent anterior instability from a traumatic etiology
- Initial traumatic anterior instability in a high-level athlete or high-demand work activities.
Arthroscopic Anterior Instability Repair Contraindications
- Large Hill Sachs lesion
- Bony Bankart lesion representing >25% of glenoid surface
- Poor-quality ligament or labral tissues
- Atraumatic, voluntary subluxation in patients with psychological problems
- Patients who will be non-compliant with post-op rehab and limitations.
- Connective tissue disorders: Ehlers-Danlos, Marfan syndrome
- Uncontrolled seizure disorder (epilepsy)
- Instabtilty associated with paresis of the deltoid, rotator cuff and/or periscapular musculature
Arthroscopic Anterior Instability Repair Alternatives
- Open Bankart Repair: Gold standard with 95-97% success rate (Andrews JR, Oper Tech Orthop 2001;11:9). 29 year follow-up demonstrates 40% osteoarthritis, 10% recurrence (Pelet S, JSES 2006:15:203).
- Non-operative treatment: physical therapy
Arthroscopic Anterior Instability Repair Pre-op Planning / Special Considerations
- Ensure adequate anchors are available including any instrumentation needed for their insertion. Generally 3.0mm or smaller bioabsorbable or metallic suture anchors are utilized.
- For patients with engaging Hill-Sachs lesions consider grafting defect arthrscopically using synthetic bone plugs (Smith& Nephew), or Arthroscopic Hill-Sachs remplissage with arthroscopic posterior capsulodesis and infraspinatus tenodesis. (AAOSNow June2007)
- Use 3-4 anchors
- Incorporate inferior and posterior tissue, not just anterior
- Lateral decibuts position has lower recurrence than beach chair.
Arthroscopic Anterior Instability Repair Technique
- Pre-operative antibiotic.
- GETA +/- scalene block.
- Lateral decubitus position, all bony prominences well padded.
- Prep and drape.
- Shoulder Examination under anesthesia. Loss of >5° of ER at 90° abduction in the affected shoulder indicates possibility of medially healed Bankart lesion (Deutsch A, Arthroscopy 2006;22:710).
- Arm is placed in sterile arm holder with 10 - 15lbs of traction. Arm postioned in 25 degrees of forward flexion, 30° abduction.
- Perform standard Shoulder Arthroscopy. Evaluate Hill-Sachs defect if present. If the defect articulates with the glenoid with the humeral head centered in less than 40 degrees of external rotation, bone grafting of the defect is indicated. Evaluate entire labrum to ensure associated SLAP Repair, or posterior / inferior labral tears are not present.
- Establish anterior-superior portal just medial to the anterolateral corner of the acromion, entering the joint just anterior to the biceps tendon.
- Establish anterior-medial portal lateral to coracoid process entering just superior to subscapularis tendon.
- Using both anterior portals elevate the labroligamentous complex from the glenoid neck to the 6 o'clock position. Ensure that the labroligamentous complex can be brought back to their anatomic positions.
- Prepare the glenoid to a bleeding bone bed using a shaver or burr.
- Mark glenoid rim at 3 and 6 o'clock postions with cautery for orientation while viewing from posterior portal.
- Move arthroscope to the anterosuperior portal.
- Anchors are then placed and capsulolabral tissue repaired as indicated. Ideal anchor position is just on the glenoid face at an angle of 45 degrees to the glenoid in a lateral-to-medial direction. Anchors should be 3.5mm or smaller in diameter.
- One limb of the suture is then passed out the posterior portal.
- Using a suture passing instrument (Suture pass, Spectum, etc) a passing suture is place through the labroligamentous tissue using the anteromedial portal and out the posterior portal. The posterior limb of the suture is then passed throught the tissue and out the anteromedial portal.
- The suture is tied using an arthroscopic sliding knot.
- Place subsequent anchors as indicated.
Arthroscopic Anterior Instability Repair Complications
- Recurrence / failure
- Hardware failure / Anchor pull-out
- Infections
- Stiffness
- CRPS
- Nerve injury: Axillary Nerve Palsy, Brachial Plexus Palsy
- Fluid Extravasation:
- Chondrolysis: though to be related to heat from electo cautery or radiofrequency probes used during capsular release or capsular shrinkage.
- Hematoma
- Chondral Injury / arthritis
Arthroscopic Anterior Instability Repair Follow-up care
- Post-Op:Shoulder immobilizer/sling. Begin pendelum ROM, elbow/wrist/hand exercises immediately.
- 7-10 Days: continue shoulder immobilizer/sling for 4-6weeks.
- 4-6 weeks: Start Physical therapy, active assist and active ROM; No external rotation past 40°. Wean from shoulder immobilizer.
- 3 Months: Progess with ROM and begin strengthening, start sport specific training.
- 6 Months: Return to sport if patient has full ROM, near full strength and no apprehension.
- Anterior-Inferior Instability Rehab Protocol.
Arthroscopic Anterior Instability Repair Outcomes
Arthroscopic Anterior Instability Repair Review References
- Burkhart SS, A Cowboy's Guide to Advanced Shoulder Arthroscopy, 2006
- Delee and Drez Orthopedic Sports Medicine, 2nd ed, 2003
- Zuckerman JD editor, Advanced Reconstruction: Shoulder, AAOS 2007
- Lee D, Operative Techniques: Shoulder and Elbow Surgery: Book, Website and DVD, 1e, 2010

- Craig EV, The Shoulder (Master Techniques in Orthopaedic Surgery), 2012
- Williams GR, Operative Techniques in Shoulder and Elbow Surgery, 2010
- Zuckerman JD, Advanced Reconstruction Shoulder (American Academy of Orthopaedic Surgeons), 2007

- Burkhart SS, The Cowboy's Companion: A Trail Guide for the Arthroscopic Shoulder Surgeon, 2012
- Burkhart SS, Burkhart's View of the Shoulder: A Cowboy's Guide to Advanced Shoulder Arthroscopy, 2006
- AANA Advanced Arthroscopy: The Shoulder: Expert Consult: Online, Print and DVD, 1e, 2010
- Gartsman GM, Shoulder Arthroscopy, 2e, 2008
- °
|