|

|
synonyms: elbow arthroscopy, elbow scope, EATS
Elbow Scope CPT
Elbow Scope Indications
- Elbow pain with abnormal PE or xray
- Loose body (snapping, clicking, locking)
- Synovial biopsy for persistent synovitis
- Elbow arthritis (osteophyte removal)
- Symptomatic plica
- Elbow contracture (capsular release)
- Lateral epicondylitis
- Elbow fracture (radial head, coronoid, capitellum)
- Evaluation of valgus instability in overhead athletes
- Posteromedial Elbow Impingement(generally a result of chronic valgus instability in the overhead athlete)
- Capitellar OCD
Elbow Scope Contraindications
- Significant prior trauma
- Active infection (arthroscopy may be of benefit in the treatment of a septic elbow)
- Elbow pain with no other supporting clinical or radiographic abnormalities
Elbow Scope Alternatives
Elbow Scope Pre-op Planning / Special Considerations
- Instrumentation needs: 4.0mm scope (consider 2.7mm for small elbows), nonvented cannulas, shaver, positioner, pump, retractors
Elbow Scope Technique
- Sign operative site
- Pre-operative antibiotics, +/- regional block (regional block can complicate post-operative NV exams).
- General endotracheal anesthesia
- Examination under anesthesia. Examine ulna nerve to ensure it does not subluxate from the cubital fossa (occurs in @16% of general population; subluxation puts ulnar nerve at risk during anterior medial portal creation).
- Lateral decubitus position with tourniquet, elbow flexed to 90° and supported with padded bulster. All bony prominences well padded, axillary role placed.
- Tourniquet placed high on the arm.
- Prep and drape in standard sterile fashion.
- Arm exasguinated with eschmar bandage. and tourniquet inflated.
- Forearm wraped with elastic bandage (Coban) to minimize extravasation.
- Distend elbow joint with saline (Normal capacity of elbow joint=15-25ml) using spinal needle in mid-lateral portal. 6cc in stiff elbows. (Galley SH, Arthroscopy 1993;9:9).
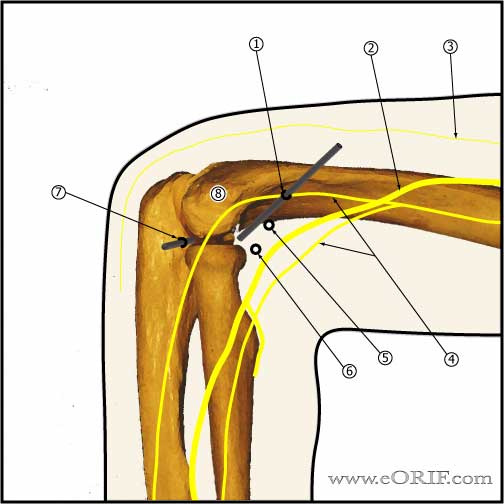
- Superomedial portal (proximal anteromedial portal): anterior to the intermuscular septum, 2cm proximal to the medial epicondyle. Must stay anterior to the medial intermuscular septum to avoid ulnar nere injury.
- Inspect anterior compartment: capitellum, radial head, rotate forarm to fully evaluate radial head, anterior capsule, lateral capsule, trochlea, coronoid fossa, coronoid process.
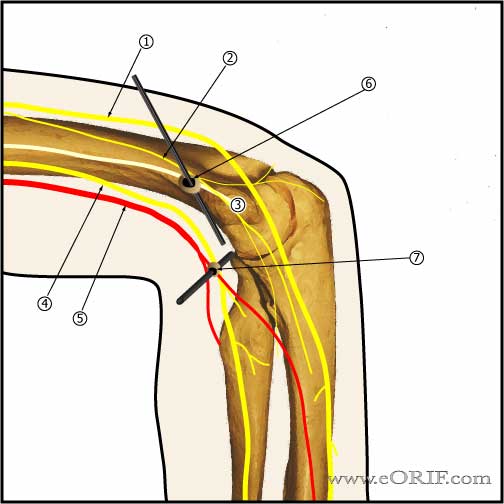
- Proximal anterolateral portal: 2cm proximal and 1cm anterior to the lateral epicondyle. Lowest risk or radial nerve injury. (MIller C, JSES 1995;4:168).
- Anterolateral portal=access to anterior joint (trochlea, coronoid process, coronoid fossa, medial radial head), placed exactly in the sulcus felt between radial head and capitellum anteriorly, elbow flexed 90°, capsule fully distended to displace NV structures anteriorly. Risks radial nerve.
- Mid-lateral portal: within soft spot in triangle formed by olecranon, lateral epicondyle, and radial head. Allows visualization of: inferior capitellum, inferior radioulnar joint. Risks:posterior antebrachial cutaneous nerve.
- Posterolateral portal=anywhere posterior to the mid-lateral portal, used for loose body removal, instrument insertion. Generally 2-3cm proximal to the tip of the olcranon along the lateral border of the triceps. Allows visualization of: olecranon tip olecranon fossa, posterior trochlea. Risks: medial and posterior antebrachial cutaneous nerves.
- Posterocentral portal=3cm proximal to the tip of the olecranon in the midline. Allows evaluation of the posterior compartment, medial gutter, lateral gutter. Risks: posterior antebrachial cutaneous nerve, ulnar nerve.
- Anteromedial portal-generally used to augment superomedial portal. Ensure ulnar nerve is not subluxed before establishing anteromedial portal. Generally 2cm distal and 2 cm anterior to the medial epicondyle. Risks: ulnar nerve, medial antebrachiocutaneous nerve.
- Posteromedial portal=no such thing, ulnar nerve is at to much risk.
- Arthroscopic valgus instability test: apply valgus stress with elbow in 70° of flexion with visualizing the medial ulnohumeral joint. Any opening >1mm indicates valgus instability.
- DJD technique: removal all loose bodies and impinging osteophytes. Consider removal of tip of the coronoid. May need capsular release.
- Chronic Valgus instability technique: perfrom arthroscopic valgus instability test, posterior osteophyte debridement, olcranon tip excision, posteromedial gutter decompression, consider olecranon fossa fenestration / deepening.
Elbow Scope Complications
- 11% minor complications, 0.8% major (Kelley EW, JBJS 2001;83A:25).
- Overall approximately 10% complication rate
- Compartment syndrome
- Septic arthritis / infection: 0.8% (Kelley EW, JBJS 2001;83A:25).
- Nerve injury (median, ulnar, radial, posterior interosseous): use of retractors effectively decreases risk.
- Cutneous neuromas (associated with portal placement).
- 4%transient radial-nerve palsy after intraarticular anesthetic injection
- Vascular injury
- Prolonged drainage (portal sites): 4% aseptic drainage
- Stiffness / flexion contracture
Elbow Scope Follow-up care
- Post-op: compressive dressing, elevation
- 1 week: Start PT focused on ROM and strengthening. AAROM, PROM. AROM, free weights start at 3 weeks.
- 6 weeks: progressive sport specific activity.
- 3 months: Return to sport / full activities.
- Elbow Arthroscopy Rehab Protocol
- Elbow Outcome Measures
Elbow Scope Outcomes
Elbow Scope Review References
- O’Driscoll, JBJS 1992;74A:84
- Abboud JA, JAAOS 2006;14:312
|