|









|
Muscles of the Anterior Thigh
| |
Muscle |
Innervation |
Origin |
Insertion |
Action |
| 1 |
Vastus lateralis |
femoral |
iliotibial line/greater trochanter/lateral linea aspera |
lateral patella |
Extend knee |
| 2 |
Vastus medialis |
femoral |
iliotibial line/medial linea aspera/supracondylar line |
medial patella |
Extend knee |
| 3 |
Vastus intermedius |
femoral |
Proximal anterior femoral shaft |
patella |
Extend knee |
Muscles of the Posterior Thigh
| |
Muscle |
Innervation |
Origin |
Insertion |
Action |
| 1 |
Biceps(long head) |
tibial |
medial ischial tuberosity |
fibular head.lateral tibia |
Flexes knee, extends hip |
| 2 |
Biceps(short head) |
peroneal |
lat linea aspera/lat intermuscular septum |
lateral tibial condyle |
Flexes knee |
| 3 |
Semitendinosus |
tibial |
Distal med. Ischial tuberosity |
anterior tibial crest |
Extends hip, flexes knee |
| 4 |
Semimembranosus |
tibial |
proximal lat ischial tuberosity |
oblique popliteal ligament/posterior capsule/posterior, medial tibia/popliteus |
Extends hip, flexes knee |
Popliteus Muscle
- Origin: Posterior aspect of tibia
- Insertion: lateral femoral epicondyle distally (11 mm) and either anterior or posterior (mean 0.84 mm anterior) to the lateral collateral ligament. (Brinkman JM, JBJS 2005;87Br:1364).
- Function: Primary function is to externally rotate the femur allowing flexion when the knee is loaded. Also: resists excessive external rotation of the tibia during knee flexion from 20 to 130 degrees; resists excessive varus rotation of the tibia during flexion from 0-90 degrees (Nielsen S, Arch Orthop Trauma Surg 1986;104:357-62); restricts posterior tibial translation; functions as a dynamic internal rotator of the tibia.
Popliteal Artery
- lies anterior to the popliteal vein and 9mm posterior to the posterior aspect of the tibial plateau when the knee is in 90° of flexion.
Biceps Femoris
- Consists or long head and short head.
- Insertion: Primarily fibular head, but also sends attachements to the ITB, Gerdy's tubercle, LCL and posterolateral capsule.
- Function: flexes knee and hip, dynamic external rotator of the tibia and lateral knee stabilizer.
- (Terry GC, AJSM 1996;24:2).
Tibial Nerve
- Origin: L4-L3, Sciatic Nerve
- Travels deep to the long head of the biceps muscle in the thigh. Splits the two heads of the gastrocnemius and travels deep to the soleus in the leg.
- Terminates as the medial and lateral plantar nerves after ig curves around the medial malleous
- Innervates: Semitendinosus, Semimembranosus, Gastrocnemius, Soleus, Plantaris, Popliteus, Flexor hallucis longus(FHL), Flexor digitorum longus(FDL), Tibialis Posterior
Common Peroneal Nerve
- Origin: L4-S2, Sciatic Nerve
- Travels laterally in popliteal fossa between the medial border of the biceps and the lateral head of the gastroc. Winds around the neck of the fibula, deep to the peroneous longus.
- Terminates as the superficial and deep peroneal nerves.
Superficial Peroneal Nerve
- Origin: Common peroneal nerve
- Travels between lateral and anterior compartments of the leg.
- Terminates as medial dorsal and intermediate dorsal cutaneous nerves
- May become entraped against its fascial opening in the distal leg. (Styf J, JBJS 1989;71B:131).
- Innervates: Peroneus longus, Peroneus brevis.
Deep Peroneal Nerve
- Origin: Common peroneal nerve
- Travels along the anterior surface of the interosseous membrane.
- Terminates as a cutaneous nerve supplying sensation to the first web space.
- Innervates: Tibialis Anterior, Extensor Hallucis longus, Extensor digitorum longus(EDL), Peroneus tertius, Extensor digitorum brevis(EDB)
Saphenous Nerve
- Origin: L3,L4, the terminal branch of the femoral nerve.
- Supples sensation to the medial knee, lower leg and ankle.
- Runs out the adductor canal, down the posteromedial knee, emerging between the sartorious and gracilis tendons.
- Lies immediately superficial to the gracilis at the posteromedial joint line.
- Can be injured during hamstring tendon harvest. (Bertram C, Arthroscopy 2000;16:763)
- Infrapatellar branch of saphenous nerve is commonly injured during medial arthrotomies resulting in medial knee numbness.
- Saphenous neuropathy: neuropathic pain or numbness in the medial knee, calf and ankle. No motor or reflex abnormalities Diagnosis can be confirmed with anesthetic blockade causing pain relief, or EMG. Can be treated with steriod injection, neurolysis or neurectomy (Worth Rm, AJSM 1984;12:80).
Sartorial Branch of the saphenous nerve
- Lies posterior to the sartorious. It is anterior to the semitendinosis with the knee in extension.
- Dissections during medial meniscal repair should remain anterior to the sartorius
- Dunaway DJ, Arthroscopy 2005;21:547
Infrapatellar Branch of the Saphenous nerve
- Exits the adductor canal on its way to the anteromedial aspect of the knee.
Iliotibial Band
- Origin: supracondylar tubercle of the femur.
- Insertion: Gerdy's tubercle of tibia, patella, patellar ligament, supracondylar tubercle.
- Function: important stabilizer of the lateral knee.
ACL Anatomy (Anterior Cruciate Ligament)
- Origin: Lateral wall of the intercondylar notch at its posterior aspect (Arnoczky CORR 1983;172:19)
- Insertion: Oval shaped area, anterior aspect of the tibial plateau between the tibial eminences. (Arnoczky CORR 1983;172:19)
- Function: Primary restraint to anterior tibial translation (90%); Secondary restraint to tibial rotation; Minor secondary restraint to varus-valgus angulation at full extension.
- Blood supply: Middle genicular artery which arises from popliteal A. The inferior medial and lateral genicular A also vascularize the ACL via the fat pad. (Arnoczky SP, Orthop Clin North Am 1985;16:15)
- Innervation: Posterior articular nerve (a branch of the tibial nerve) (Kennedy JC, JBJS 1974;56A:223). Normal ACL has proprioceptive senses that help protect the knee joint during use which are lost after reconstruction.
- Length = 31-38mm, Width = 11mm (Girgis CORR 1975;106:216) (Odenstein JBJS AM 1985;67:257)
- Anteromedial portion is tighter in flexion, posterolateral portion is tighter in extension
- Intracapsular, but extrasynovial
- Tensile strength = 2,150 N, stiffness = 242 N/mm. Tension forces in the ACL are highest with the knee in full extension (Markolf KL, JBJS 1996;78A:1728).
- Composition: Type I collagen (90%), Type III collagen (10%)
- See also ACL Tear.
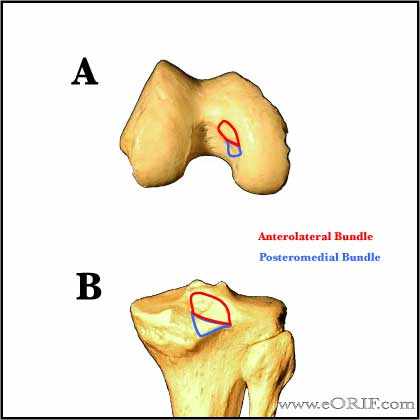
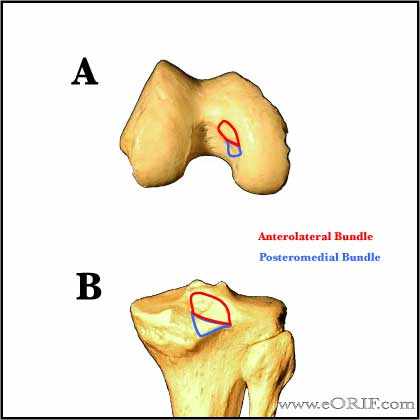
PCL Anatomy (Posterior Cruciate Ligament)
- Origin: Broad crescent-shaped area on the anterolateral aspect of the medial femoral condyle. (Girgis FG, CORR 1975:216-231).
- Insertion: Posterior tibia, below the articular surface. (Girgis FG, CORR 1975:216-231).
- Function: PCL is responsible for 95% of total restraint to posterior translation of the tibia. Secondary restraint to tibial external rotation. In the PCL deficient knee posterior tibial translation is greatest at high flexion angles and is increased with sectioning of the posterolateral corner, MCL and posteromedial structures. (Noyes FR, AJSM 1993;21:407).
- Blood Supply: Middle genicular artery which arises from popliteal A. The inferior medial and lateral genicular A also vascularize the PCL via the fat pad. (Arnoczky SP, Orthop Clin North Am 1985;16:15)
- Innervation: Posterior articular nerve (a branch of the tibial nerve) (Kennedy JC, JBJS 1974;56A:223). Normal PCL has proprioceptive senses that help protect the knee joint during use which are lost after reconstruction.
- Consists of an anterolateral portion (tight in flexion) and a postermedial portion (tight in extension.)
- Length: 38mm; Width: 13mm.
- See also PCL tear.
LCL Anatomy (Lateral Collateral Ligament)
- Origin: posterior (4.6 mm) and proximal (1.3 mm) to the lateral femoral epicondyle posterior and superior to the insertion of the poplitieus. (Brinkman JM, JBJS 2005;87Br:1364).
- Insertion: posterior (8.1 mm) to the anterior point of the head of the fibula. (Brinkman JM, JBJS 2005;87Br:1364).
- Function: Primary restraint to varus stress of the knee. Resists tibial external rotation. Section the LCL increases external rotation at 30°. External rotation of the tibia is highest after sectioning the LCL and PCL with the knee at 90° flexion. (Gollehon DL, JBJS 1987;69A:233).
- Tight in extension, lax in flexion.
- See alsoLCL Tear.
MCL Anatomy (Medial Collateral Ligament)
- Composed of superficial and deep fibers. (Satterwhite Y, Op Tech Sports Med 1996;4:134) (Warren RF, JBJS 1979;61A:56).
- Origin: Superficial MCL=medial femoral epicondyle
- Insertion: Superficial MCL=periorsteum of proximal tibia, deep to the pes anserinus.
- Function: Primary restraint to valgus instability.
- Blood Supply:
- Deep MCL is a capsular thickening.
- More commonly injury at is femoral origin than tibial insertion.
- See also MCL tear.
Popliteofibular Ligament
- Origin: distal (1.3 mm) and anterior (0.5 mm) to the tip of the styloid process of the fibula. (Brinkman JM, JBJS 2005;87Br:1364).
- Insertion: joins popliteus tendon to insert into the lateral femoral epicondyle.
- Function: static stabilizer of the lateral and posterolateral knee resisting varus rotation and posterolateral tibial rotation and posterior tibial translation. (Maynard MJ, AJSM 1996;24;311)
Arcuate Ligament
- Origin: fibular styloid process
- Insertion: lateral femoral condyle
- Function: reinforces posterlateral capsule, covers the popliteus.
Ligament of Humphrey: (anterior meniscofemoral ligament)
- Origin: posterior horn of the lateral meniscus, runs anterior to the to the PCL
- Insertion: distal edge of the femoral PCL attachment
- 70 % of knees have either anterior meniscofemoral ligament of Humphrey or posterior meniscofemoral ligament of Wrisberg.
Ligament ofWrisberg: (posterior meniscofemoral ligament)
- Origin: posterior horn of lateral meniscus.
- Insertion: medial femoral condyle
- 70 % of knees have either anterior meniscofemoral ligament of Humphrey or posterior meniscofemoral ligament of Wrisberg.
Posterolateral Corner Anatomy
- Posterolateral Complex includes: biceps tendon, iliotibial band, popliteus tendon, poplitoefibular ligament, arcuate ligament and the LCL. (OKU-8)
- PLC Function: restraint to posterior tibial translation, varus rotation and external tibial rotation.
- Some also consider it to include: the middle third of the lateral capsular ligament, the fabellofibular ligament, the posterior horn of the lateral meniscus, the lateral coronary ligament, and the posterolateral part of the joint capsule. (Covey D, JBJS 2001;83A:106-118)
- Majority of injuries are distally based disruption of tissues from fibula and proximal lateral tibia.
- See also Posterior lateral corner injury
Medial Patellofemoral Ligament
- Origin: Adductor tubercle of the distal femur: medial epicondyle immediately superior to the attachment of the medial collateral ligament. (Steensen RN, AJSM 2004;32:1509).
- Insertion: superomedial border of the patella via a wide insertion: @1 cm distal to the superior pole of the patella, near the widest portion of the patella. (Steensen RN, AJSM 2004;32:1509).
- Courses deep to the retinaculum in layer II; deep to the sartorius and is partially cavered by the Vastus medialis.
- Function: Provides 50%-60% of the resistance to lateral displacement of the patella.
- Mean length = Mean width+ (Amis A, Knee 2003;10:215).
- Strength = 208 N (Moutney J, JBJS 2005;87Br:36).
- >94% of Patellar Dislocation are related to MPFL rupture.
Meniscus Anatomy
- Medial meniscus: C-shaped; anterior horn attaches ?; posterior horn attaches anterior to the insertion of the posterior cruciate ligament. (Johnson DL, Arthroscopy 1995;11:386) Average length = 45.7mm (McDermott ID, Knee Surg Sports Traumatol Arthrosc 2004;12:130). Secondary stabilizer to anterior tibial translation.
- Lateral Menisus: semicircular; anterior horn attaches adjacent to the ACL; posterior horn attaches behind the intracondylar eminence.(Johnson DL, Arthroscopy 1995;11:386) Average length = 35.7mm (McDermott ID, Knee Surg Sports Traumatol Arthrosc 2004;12:130).
- Discoid variant of the lateral meniscus is found in 3.5% to 5% of patients. (Vandermeer RD, Arthroscopy 1989;5:101)
- Average excursions of the menisci with knee flexion = 5.2 mm for the medial and 11 mm for the lateral meniscus. (Thompson WO, AJSM 1991;19:210)
- Medial meniscus transmits 50% of the load in the medial compartment. Lateral meniscus transmits 70% of the load in the lateral compartment. (Greis PE, JAAOS 2002;10:168). Degenerative changes occur earlier in pts undergoing parital lateral meniscectomy than partial medial meniscectomy.
- Blood supply: the outer 10% to 30% has blood supplied from the perimeniscal capillary plexus off the superior and inferior medial and lateral genicular arteries. (Arnoczky SP, AJSM 1982;10:90)
- Medial and lateral menisci are attached by the transverse (intermeniscal) ligament and posteriorly by the coronary ligaments
- see also Meniscal Tear.
- see also Medvecky MJ, JAAOS 2005;13:121
Knee Anatomy Review References
- Medvecky MJ, JAAOS 2005;13:121
- °
|