|


|
synonyms: baseball finger, drop finger, finger extensor tendon avulsion
Mallet Finger ICD-10
Mallet Finger ICD-9
- 736.1(acquired)
- 755.59(congenital)
Mallet Finger Etiology / Epidemiology / Natural History
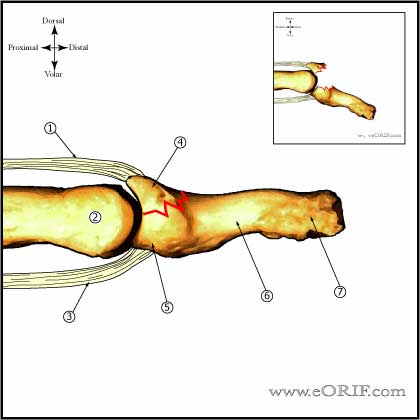
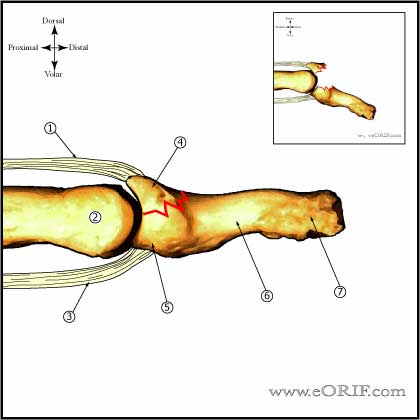
- Disruption of the extensor mechanism at the level of the DIP joint.
- Caused by forced flexion of the extended DIP joint.
- Usually involves long, ring or small fingers (Brzezienski MA Hand Clin 1995;11:373)
- Without treatment the terminal extensor tendon migrates proximally, increasing extensor tone at the PIP joint which can lead to a swan neck deformity
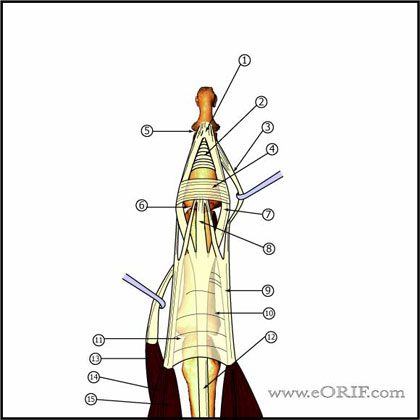
Mallet Finger Anatomy
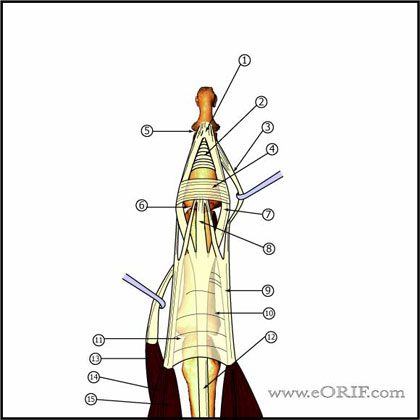
- DIP extension is provided by the the conjoined lateral bands which insert into the base of the distal phalanx
- Conjoined lateral bands are made up of the lateral slips of the extrinsic extensor tendon and the lateral bands from the intrinsic interosseous and lumbrical muscles.
Mallet Finger Clinical Evaluation
- Pain, inability to extend DIP joint
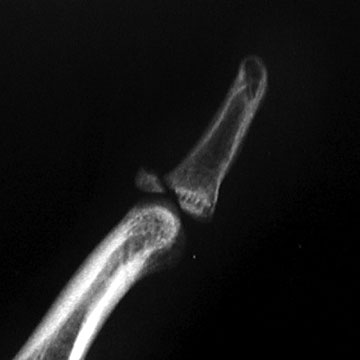
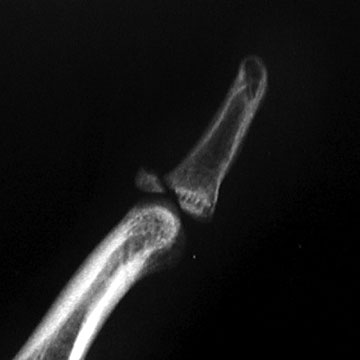
Mallet Finger Xray / Diagnositc Tests
- P/A, oblique, and lateral radiographs of finger. Often normal, may show avulsion fragment, or articular fracture.
Mallet Finger Classification / Treatment
- Closed No fracture or fracture involving <1/3 of the articular surface = involved digit immobilized in full extension or hyperextension across the DIP joint. PIP joint is generally not immobilized. Maintain for 8weeks, followed by nightime splint use for 2-3 weeks. Splinted period must be restarted if patient inadvertently flexes finger during treatment period. (Okafor B, JBJS 1997;79B:544) Full time extension splinting for 8 wks even up to 6 months after terminal extensor tendon rupture leads to good results in the vast majority of patients. Surgery is rarely necessary.
- Open = lacerations are generally repaired with running suture reapproximating both skin and tendon +/-longintudinal K-wire fixation of DIP joint in extension.
- Closed with fracture >1/3 of articular surface / DIP joint subluxation = closed reduction with Extension Block Pinning 26756. (Tetik C, Clin Orthop 2002;404:284-290), (Pegoli L, J Hand Surg 2003;28B:15)
- Chronic injuries (generally those > 6months old, or have failed extension splinting) = consider tenodermodesis (Iselin F, J Hand Surg 1977;2Am:118); oblique retinacular ligament reconstruction (Kleinman WB, J Hand Surg 1994;9Am:399); DIP fusion
Mallet Finger Associated Injuries / Differential Diagnosis
Mallet Finger Complications
- skin maceration/ulceration
- tape allergy
- infection
- nail plate deformity
- hardware failure
- DIP joint deformity
- pain
Mallet Finger Follow-up Care
- Post-op /Initial: Place in alumifoam extension / clamshell / Stack splint. Elevation.
- 7-10 Days: xray to ensure reduction is maintained. Continued splint, activity modifications. Immobilize as few joints as necessary.
- 6 Weeks: Remove k-wire, wean from splint use as soon as callus is visible on xray. Continue activity modifications. Agressive DIP ROM.
- 3 Months: Resume full activities. Assess ROM.
- 1Yr: assess outcomes / follow-up xrays.
Mallet Finger Review References
- Bendre AA, JAAOS 2005;13:336
- Wehbe MA, Schneider LH: Mallet fractures. J Bone Joint Surg 1984;66A:658-669.
- Stern PJ, Kastrup JJ: Complications and prognosis of treatment of mallet finger. J Hand Surg 1988;13A:329-334.
- Garberman SF, Diao E, Peimer CA: Mallet finger: Results of early versus delayed closed treatment. J Hand Surg 1994;19A:850-852.
- Rockwood and Green's Fractures in Adults 6th ed, 2006°
|