 |
synonyms: multi-directional instaiblity of the shoulder
MDI Arthroscopic Plication CPT
MDI Arthroscopic Plication Indications
- Failed non-operative management of MDI
MDI Arthroscopic Plication Contraindications
- Emotional/psychological problems
- Congenital glenoid aplasia
- Hypoplasia
- Non-compliance with therapy
- Workman’s comp
- Axillary/suprascapular nerve injury
MDI Arthroscopic Plication Alternatives
- Open anterior-inferior Capsular shift (Pollock RG, JBJS 2000:82:919).
- Thermal capsular shrinkage: risks chondrolysis (Levine WN, JBJS 2005;87A:616), capsular thinning / recurrent instability (Park HB, AJSM 2005;33:1321).
MDI Arthroscopic Plication Planning / Special Considerations
- Essential components=rotator interval closure & reduction of joint volume
- Goal: FE=160, IR=T-8, ER=30 degrees
- Closure of the rotator interval has not been definitively shown to enhance stability or improve outcomes for patients with MDI.
MDI Open Technique
- Sign operative site.
- Pre-operative antibiotics, +/- regional block.
- EUA
- Beach chair, eye patches, bony prominences well padded, arm prepped and draped
- standard axillary incision from coracoid to axilla, in the anterior axillary fold
- inject 1% lido with epi along incision
- cephalic vein, deltopectoral interval
- cephalic vein preserved and taken laterally with deltoid(repair cephalic vein lacs with 8-0 nylon)
- can release proximal 1-2cm of pectoralis insertion for improved inferior exposure.
- Richardson retractors to reflect deltoid laterally, pec medially
- incised clavipectoral fascia just lateral to conjoined tendon.
- axillary nerve palpated by sliding finger along anterior border of subscapularis. Should be at @ 6o’clock position.
- retract conjoined tendon to expose subscapulairs
- anterior humeral circumflex vessels preserved(on inferior third of subscapularis tendon)
- small Darrach retractor placed in rotator interval
- proximal 2/3 of subscapularis incised 1.5-2cm from lesser tuberosity insertion
- subscapularis tendon reflected off anterior capsule
- horizontal incision in line with tendon fibers separating proximal 2/3 form distal 1/3. Distal 1/3 preserved.
- #2 Ethibond placed in subscap tendon
- inferior subscap reflected form capsule with periosteal elevator
- Scoffield retractor placed in interval protecting axillary nerve
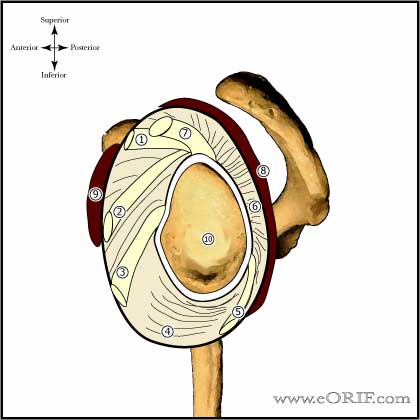
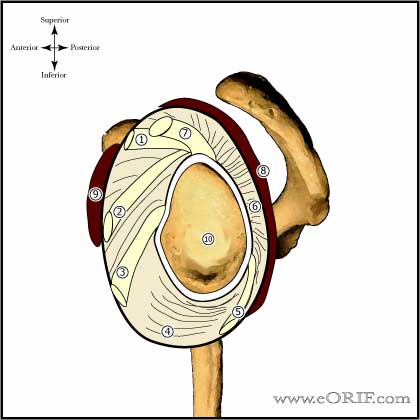
- capsule exposed from 12o’clock to 6o’clock position
- anterior capsule incised midway between glenoid and humeral attachments from rotator interval to 6 o’clock position
- horizontal mattress sutures placed in medial capsule, sutures exit extra-articular
- retract medial capsule to exposed glenoid rim; evaluate for Bankart lesion decorticate anterior glenoid with bur
- 2-3 suture anchors placed from 2-6o’clock for right shoulder, 10-6o’clock for left shoulder
- Rowe or Fukuda retractor pushing HH posteriorly may aid exposure.
- any rotator interval defect repair/closed
- medial capsule shifted laterally and superior beginning with most inferior suture.
- inferior sutures tied at abducted 90, ER 50
- middle suture tied at abducted 45 ER 40
- superior sutures tied at arm at side ER 30
- check ROM
- irritation
- repair subscapularis using previously placed stay sutures, repair horizontal defect with #2 ethibond
- check ROM
- irrigate
- palpate Axillary nerve
- SQ closed with 2-0 inverted interrupted Vicryl
- skin closed with 3-0 running SQ stich
- mastisol, steri-strips-zerofrom-4x4-ABD-foam tape-shoulder immobilizer
MDI Arthroscopic Plication Complications
- Neurologic injury; 8.2% incidence after anterior reconstruction for recurrent GH instability. 78% recover completely. (Ho E, JSES 1999;8:266-270). Axillary nerve, Brachial plexus
- Loss of ER, with eventual GH DJD.
- Recurrent MDI
- Pain
- Hardware failure / Anchor pull-out
- Infections
- Stiffness
- CRPS
- Fluid Extravasation:
- Chondrolysis: though to be related to heat from electo cautery or radiofrequency probes used during capsular release or capsular shrinkage.
- Hematoma
- Chondral Injury / arthritis
- Instrument failure
- Weakness
MDI Arthroscopic Plication Follow-up care
- Post-op: shoulder immobilizer, remove dressing at 72 hrs, replace dressing, may shower if dry, replace dressing after each shower.
- 7-10 Days: Pendelum exercises, passive FE with overhead pulley, gentle passive ER with a stick 4-6 times daily. Limit of ER is determined at surgery. Elbow wrist hand ROM. Sling contiuously for 2-3 weeks, with activity thereafter.
- 6 Weeks: Advance to stregthening. Full active ROM.
- 3 Months: Sport specific training.
- 6 Months: Return to sport/heavy labor at 5-8months depending on regaining 90% of strength.
- 1Yr: Mid-range stability is mainly dependent on muscular balance and coordination. Lifelong rehab program is required.
- Shoulder Outcome measures
MDI Arthroscopic Plication Outcomes
- Arthorscopic Capsular Plication: 97% good/excellent results (Kim SH, AJSM 2004;32:594).
- Nonsurgically treated young, athletic patients: 49% significant pain, 46% continued instability, 37% go on to have surgical treatment. By the modified Rowe grading scale 14% excellent results, 33% good, 53% poor results. (Misamore GW, JSES 2005;14:466).
MDI Arthroscopic Plication Review References
- Burkhart SS, A Cowboy's Guide to Advanced Shoulder Arthroscopy, 2006
- Rockwood and Green's Fractures in Adults 6th ed, 2006
- OKU - Shoulder and Elbow 2nd ed, 2002°
- Tjoumakaris FP, Bradley JP. The rationale for an arthroscopic approach to shoulder stabilization. Arthroscopy. 2011 Oct;27(10):1422-33. Epub 2011 Aug 26.
- Gaskill TR, Taylor DC, Millett PJ. Management of multidirectional instability of the shoulder. J Am Acad Orthop Surg. 2011 Dec;19(12):758-67. Review. PubMed PMID: 22134208.
|