 |
synonyms: pec major repair, pectoralis major reconstruction
Pectoralis Major Repair An
Pectoralis Major Repair Anatomy
- Pec tendon is 5 cm wide, 1 cm long on the anterior surface, and 2.5 cm long on the posterior surface. It consists an anterior lamina(clavicular head), and a posterior lamina is formed by the sternal head.
- The fascia surrounding the pectoralis major is continuous with the fascia of the brachium and the medial antebrachial septum. This fascia presents as a palpable cord in the axilla and may be mistaken for an intact pectoralis major tendon.
- Most common rupture is a tendon avulsion, but can be a rupture at the myoteninous junction, bony avulsion, tendon mid substance rupture, or muscle belly tear.
- Some consider three heads of origin: clavicular, sternal and abdominal (Wolfe SW, AJSM 1992;20:587)
Pectoralis Major Repair Indications
- Complete pectoralis major tendon rupture
- Isolated sternal head of pectoralis major rupture
- Complete pectoralis moajor rupture at eh myotendionuous juntion
Pectoralis Major Repair Contraindications
- Partial low-grade pectoralis major tendon ruptures
- Complete Sternoclavicular origin ruptures
- Pectoralis major muscle belly rupture (relative)
Pectoralis Major Repair Alternatives
- Non-operative treatment (associated with strength deficits and limited return to athletic activity for complete distal tendon tears)
Pectoralis Major Repair Pre-op Planning / Special Considerations
- Have Achilles tendon allograft available and discuss allograft use with patient pre-operatively. (Joseph TA, JSES 2003;12:101)
- Consider MRI to determine location of rupture and amount of retraction. Chronic injuries at the muscle-tendon junction that demostrate fatty infiltrate on MRI will be difficult to mobilized / repair with a successful outcome.
Pectoralis Major Repair Technique
- Pre-operative antibiotic
- Anesthesia: GETA +/- interscalene / supraclavicular block
- Postion: Modified beach chair, all bony prominences well padded.
- EUA:
- Prep and drape in standard sterile fashion.
- Deltopectoral incision. Slightly more medial proximally to access the retracted tendon. Slightly more lateral distally to access the pec major insertion.
- The anterior laminar fibers from the clavicular head, scar tissue and the anterior fascia may give the false appearance of an intact tendon.
- Bluntly dissect to the ruptured sternal portion of the pectoralis major tendon, which lies posterior and usually is retracted medial to the clavicular insertion.
- Mobilize, excise poor tissue and place stay sutures in the tendon end.
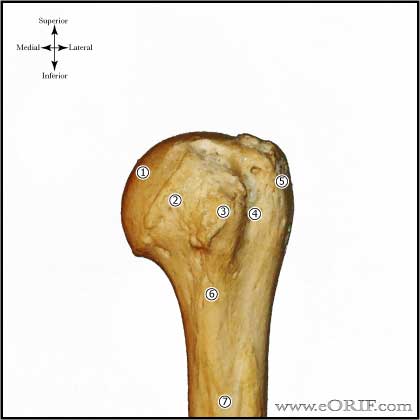
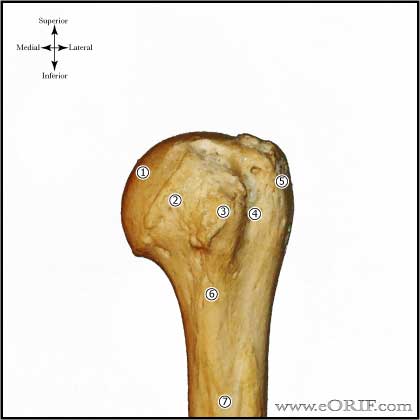
- Identified the insertion site just lateral to the long head of the biceps and lateral to the bicipital groove.
- Prepare bone bed and repair tendon to bone using bone tunnels or suture anchors. 3-5 anchors are typically required. Sutures are tied with the arm in neutral.
- Intramuscular ruptures are repaired with modified Kessler technique using Multiple no. 2 braided nonabsorbable sutures placed in three layers beginning in the posterior fascia, followed by a middlel ayer, and finally by placing a third layer through the anterior fascia and muscle. (Kragh JF Jr, JBJS 2002;84A:992)
- Irrigate
- Close in layers.
Pectoralis Major Repair Complications
- Persistent weakness
- Infection
- Myositis Ossificans
- Shoulder stiffness (abduction)
- Re-rupture / failure
Pectoralis Major Repair Follow-up care
- Post-op: Shoulder immobilizer for 4-6 weeks. Elbow/wrist/hand ROM exercises.
- 7-10 Days: Start pendulum ROM exercises.
- 6 weeks: gentle passive ROM gradually advanced to full ROM and gentle periscapular strengthening started.
- 3 months: ROM should be nearly full and Pectoralis major muscle strengthening is begun.
- 6 months: push-ups and dumbbell bench presses with light weight and high repetition are started.
- 9 to 12 months: return to full-activities. High-weight, low repetition barbell bench pressing is discouraged indefinitely.
Pectoralis Major Repair Outcomes
- Subjective ratings: 96% for acute repair, 93% for chronic repair, 51% for nonoperative treatment. (Schepsis AA, AJSM 2000;28:9)
- Isokinetic adduction strength testing: acute repair = 102% of the opposite side; chronic injury repair =94%: nonoperative treatment=71%. (Schepsis AA, AJSM 2000;28:9).
Pectoralis Major Repair Review References
Petilon J, JAAOS 2005;15:59
|