|
synonyms: phalanx fracture
Phalangeal Shaft Fracture ICD-10
A- initial encounter for closed fracture
B- initial encounter for open fracture
D- subsequent encounter for fracture with routine healing
G- subsequent encounter for fracture with delayed healing
K- subsequent encounter for fracture with nonunion
P- subsequent encounter for fracture with malunion
S- sequela
Phalangeal Shaft Fracture ICD-9
- Unspecified = 816.00 (closed), 816.10(open)
- Proximal or middle phalanx = 816.01(closed), 816.11(open)
- Distal phalanx = 816.02(closed), 816.12(open)
- Multiple sites = 816.03(closed), 816.13(open)
Phalangeal Shaft Fracture Etiology / Epidemiology / Natural History
Phalangeal Shaft Fracture Anatomy
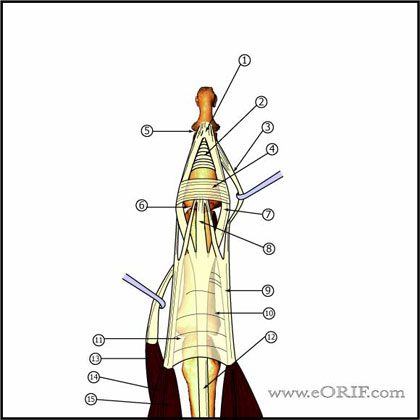
- DIP extension is provided by the the conjoined lateral bands which insert into the base of the distal phalanx
- Conjoined lateral bands are made up of the lateral slips of the extrinsic extensor tendon and the lateral bands from the intrinsic interosseous and lumbrical muscles.
- DIP flexion is provided by FDP insertion into the volar base. Injury to the FDP at this level results in a Jersey Finger.
- See Hand Anatomy.
Phalangeal Shaft Fracture Clinical Evaluation
- Evaluate finger cascade with flexion. Any overlaps of injured digits indicates need for reduction +/- fixation.
Phalangeal Shaft Fracture Xray
- P/A, lateral abd oblique views of affected finger
Phalangeal Shaft Fracture Classification / Treatment
- Undisplaced (>2mm translation, >20 degrees angulation, no clinical deformity): Treatment = static or dynamic splinting (buddy taping). Follow weekly initially to ensure reduction is maintained (Maitra A, J Hand Surg 1992;17Br:332).
- Displaced transverse or short oblique: may be stable after reduction. If stable apply static splint in functional position for 4-6weeks. Unstable = CRPP vs ORIF. Consider transcutaneous mini-screws.
- Displaced Long oblique = Almost always unstable = CRPP(CPT=26727). Consider transcutaneous mini-screws. ORIF if fails closed reduction.
- Open fracture: consider mini-external fixation. (Freeeland AE, CORR, 1987;214:93)
Phalangeal Shaft Fracture Associated Injuries / Differential Diagnosis
- Phalangeal Base Fracture
- Phalangeal Neck Fracture
- Distal Phalanx Fracture
- Mallet finger
Phalangeal Shaft Fracture Complications
- Loss of reduction
- Delayed union
- Malunion
- Nonunion
- Tendon adhesion / stiffness
- Nerve or vascular injury
Phalangeal Shaft Fracture Follow-up
- Post-op /Initial: Place in alumifoam extension / clamshell. Elevation.
- 7-10 Days: xray to ensure reduction is maintained. Continued splint, activity modifications. Immobilize as few joints as necessary.
- 6 Weeks: Remove k-wire, wean from splint use as soon as callus is visible on xray. Continue activity modifications. Agressive DIP ROM.
- 3 Months: Resume full activities. Assess ROM. May require flexor/extensor tendon tenolysis to regain motion.
- 1Yr: assess outcomes / follow-up xrays.
Phalangeal Shaft Fracture Review References
- Freeland AE, Geissler WB, Weiss AP, Operative Treatment of Common Displaced and Unstable Fractures of the Hand, JBJS 2001;83A:928-945
- Freeland AE, Orbay JL. ORIF of the Tubular Bones of the Hand In: Stickland JW, Grahma TJ, editor. Hand 2nd ed. Master Techniques in orthopedic surgery. Philadeplhia: Lippincott-Raven; 2004. p 3
- Rockwood and Greens
- Greens Hand Surgery
|