|
synonyms: Achilles tendon tear, Achilles rupture, Achilles tear Achilles Tendon Rupture ICD-10
Achilles Tendon Etiology / Epidemiology / Natural History
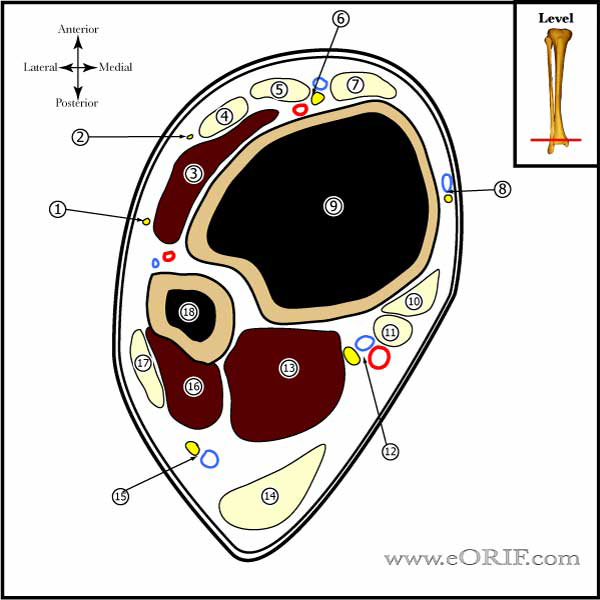
Achilles Tendon Clinical Evaluation
Achilles Tendon Xray / Diagnositc Tests
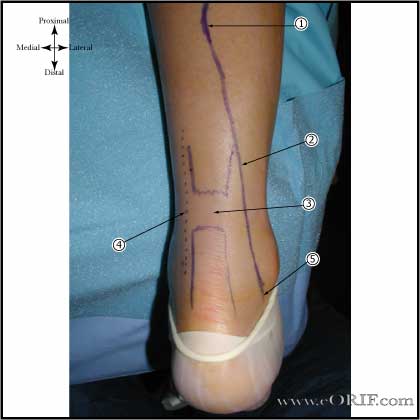
Achilles Tendon Classification / Treatment
Achilles Tendon Rupture Non-operative Treatment
Achilles Tendon Associated Injuries / Differential Diagnosis
Achilles Tendon Follow-up Care
Achilles Tendon Review References
|