|
|
synonyms: traumatic brachial plexus injury, lesions of the brachial plexus, supraclavicular injuries, upper plexus injuries, lower plexus injuries, brachial plexus palsy, upper trunk, middle trunk, lower trunk
Brachial Plexus ICD-10
- G54.0: Brachial plexus disorders
Brachial Plexus ICD-9
- 353.0 (Brachial plexus lesions; cerical rib syndrome, costoclavicular syndrome, scalenus anticus sydrome, thoracic outlet syndrome)
- 353.8 (Other nerve root and plexus disorders)
- 353.9 (Unspecified nerve root and plexus disorder)
Brachial Plexus Etiology / Epidemiology / Natural History
- Generally caused by MVA in adults. Generally males aged 15 to 25 years old.
- Rule of “seven seventies.” 70% occurr secondary to MVAx; of these 70% involve motorcycles or bicycles. Of cycle riders, 70% have multiple injuries. Overall, 70% have supraclavicular lesions; of those, 70% have at least one root avulsed. At least 70% of patients with a root avulsion also have avulsions of the lower roots (C7, C8, orT1). Of patients with lower root avulsion, nearly 70% will have persistent pain. (Narakas AO, Int Orthop 1985;9:29)
- If head is rapidly forced away from shoulder the injury is generally at C5,C6. If arm is rapidly abducted the lesion is generally at C8-T1.
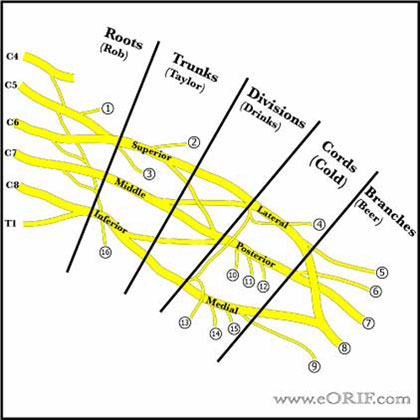
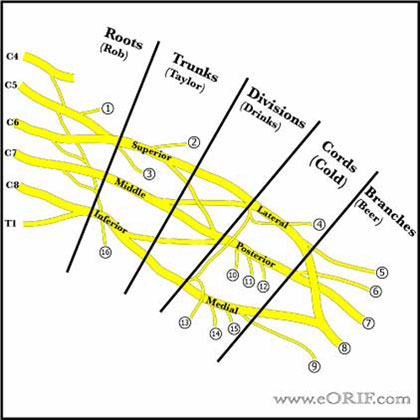
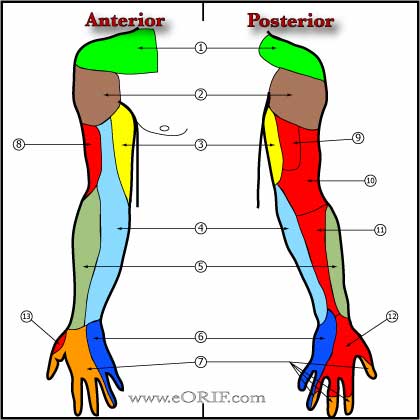
Brachial Plexus Anatomy
- Brachial plexus is formed from C5, C6, C7, C8, and T1 nerve roots. There may be contributions from C4, and T2. A plexus with contributions from C4 is called “prefixed.” (28% to 62%). "Postfixed" = contributions from T2 (16% to 73%). (Kerr AT, Am J Anat 1918;23:285).
- Roots and trunks are more commonly affected than the divisions, cords, or terminal branches.
- Trapezius and levator scapulae muscles are almost always intact after traumatic brachial plexus injury allowing for active arm abduction through the scapulothoracic articulation.
- If serratus anterior function is preserved, forward elevation of the arm through scapular rotation is possible.
- Preganglionic injury = spinal roots are avulsed from the spinal cord; little potential for recovery. Postganglionic = distal to the dorsal root ganglion; some potential for spontaneous recovery.
- Avulsion of the T1 root (a pre-ganglionic injury) interrupts the T1 sympathetic ganglion,c ausing Horner's syndrome (miosis (small pupil), enophthalmos (sinking of the orbit), ptosis (lid droop), and anhydrosis (dry eyes).
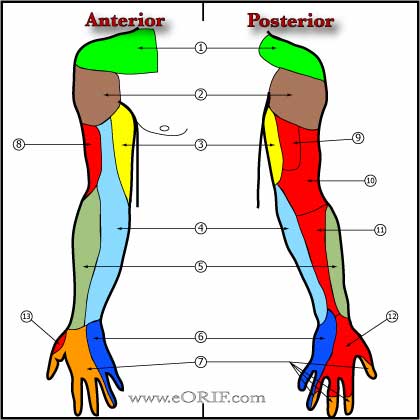
- Injury to C5,C6,C7 may result in loss of shoulder flexion, elbow fexion and extension and occasionally wrist and finger extension.
- Injury to C8 and T1 may limit hand function.
- Upper trunk = C5,C6 = rhomboids, deltoid, infraspinatus, brachioradialis.
- Middle trunk = C7 = pronator teres, extensor carpi radialis
- Lower trunk = C8 = extensor carpi ulnaris, flexor carpi ulnaris, flexor pollicis longus.
Brachial Plexus Clinical Evaluation
- Often involves poly trauma patients. Patients must be stabilized using ATLS standards first.
- Compete neurologic exam.
- Median, ulnar, and radial nerves are evaluated by examining finger and wrist motion. Elbow flexion = musculocutaneous nerve. Elbow extension = high radial nerve function. Shoulder abduction = axillary nerve(branch of posterior cord).
- Posterior cord = wrist extension, elbow extension, and shoulder abduction.
- Latissimus dorsi: innervated by the thoracodorsal nerve, a branch of the posterior cord. Palpated in the posterior axillary fold and can be felt to contract when a patient is asked to cough.
- Pectoralis major: Medial pectoral nerve (medial cord) innervates the sternal head of the pectoralis major, and the lateral pectoral nerve (lateral cord) innervates the clavicular head. Pectoralis major muscle can be palpated from superior to inferior as the patient adducts the arm against resistance.
- Suprascapular nerve is a terminal branch at the trunk level. It can be examined by assessing shoulder external rotation and elevation.
- Horner's syndrome, (miosis (small pupil), enophthalmos (sinking of the orbit), ptosis (lid droop), and anhydrosis (dry eyes), suggests a root avulsion at the C8-T1 level.
- Long thoracic nerve: formed from the roots of C5-C7. Innervates the serratus anterior muscle. Injury causes Scapular Winging as the patient attempts to forward elevate the arm.
- Dorsal scapular nerve: Formed from C4-C5. Innervates the rhomboid muscles. Injury indicted by atrophy of the rhomboids and parascapular.
Brachial Plexus Xray / Diagnositc Tests
- C-spine, shoulder (anteroposterior and axillary views), and chest views indicated. Transverse process fractures in the cervical vertebrae suggest root avulsion at the same level. Clavicle or rib fractures (first or second rib) suggest brachial plexus injury.
- CT with myelography: helping to define the level of nerve root injury. Root avulsions appear as pseudomeningoceles on CT myelogram done 3 to 4 weeks after injury. (Carvalho GA, J Neurosurg 1997;86:69).
- MRI: may show: large neuromas after trauma or associated inflammation or edema, mass lesions in patients with spontaneous nontraumatic neuropathy. (Nakamura T, JBJS 1997;79Br:764).
- EMG/NCV: best performed 3 to 4 weeks after injury. Consider serial EMG/NCV with repeat physical examination to document and quantify reinnervation or denervation. Fibrillations = denervation. Active motor units with voluntary effort and few fibrillations at rest offers a good prognosis compared with the absence of motor units and many fibrillations (poor prognosis). Preganglionic injury is indicated by denervation of cervical paraspinals, rhomboids, serratus anterior. SNAPs are preserved in lesions proximal to the dorsal root ganglia (preganglionic). SNAPs are absent in a postganglionic or a combined pre- and postganglionic lesion. Recovery is indicated by emergence of nascent potentials, a decreased number of fibrillation potentials, or the appearance of an increased number of motor unit potentials.
Brachial Plexus Classification / Treatment
- Physical therapy should be started immediately to prevent contractures and to strengthen functioning muscles.
- Sharp open injuries: Immediate exploration and primary repair of the injured portion of the brachial plexus is indicated.
- Low-velocity gunshot wounds: should be observed because most are neurapraxic brachial plexus injuries.
- High-velocity gunshot wounds: controversial, consider surgical exploration depending on amount of soft tissue injury.
- Stretch injuries: Exploration/reconstruction indicated if no/inadequate reinnervation has occured 3 to 6 months after injury. Early exploration/reconstruction (3-6 weeks) is indicated for root avulsions. Results from delayed (6 to12 months) or late (>12 months) surgery are poorer because the time for the nerve to regenerate to the target muscles is greater than the survival time of the motor end plate after deenervation.
- Burners Syndrome
- Preganglionic (supraganglionic): loss of motor function with retained sensory nerve action potentials. Treatment = neurotization.
- Postganglionic (infraganglionic): loss of motor and sensory function: generally treated with surgical repair/grafting.
- See also Pediatric Brachial Plexus Palsy.
Primary surgical options
- Direct repair: indicated for sharp injuries / lacerations. Contraindicated for stretch injuries. Consider augmentation with fibrin sealant(fibrinogen with aprotinin mixed with thrombin and calcium chloride) and neurotrophic factors (Jubran M, Exp Neurol 2003;181:204) or sural nerve graft (Seddon HJ, JBJS 1963;45Br:447).
- Neurolysis: may be performed alone when the nerve is in continuity and a NAP is obtained is obtained during intraoperative neurodiagnostic studies.
- Intraplexal Nerve grafting: indicated for ruptures or postganglionic neuromas that do not conduct a NAP across the lesion. Grafts options = sural nerve or other cutaneous
nerves.
- Surgical Priorities: (1)elbow flexion, (2)shoulder stability, (3)protective hand sensation, (4)stable wrist extension, (5)dynamic finger flexion, (6)intrinsic hand function.
- Nerve transfers / Neurotization: Transfers a functioning nerve of lesser importance to a more important denervated distal nerve. Mainly aimed at restoring elbow flexion. Should be performed within 6 months of injury. Common donor nerves = spinal accessory nerve (cranial nerve XI), intercostal nerves (motor and sensory), medial pectoral nerve, fascicle of a functioning ulnar nerve (Oberlin C, J Hand Surg 1994;19Am:232), median nerve in patients with intact C8 and T1.
- Spinal accessory or the phrenic nerve can be transfered to the suprascapular nerve for shoulder abduction. (Merrell GA, J Hand Surg 2001;26Am:303).
- Elbow flexion = intercostal nerves directly or the spinal accessory nerve with an interpositional graft directly targeting the biceps motor branch or fascicle of a functioning ulnar nerve transfered to the musculocutaneous nerve. (Oberlin C, J Hand Surg 1994;19Am:232)
- Upper trunk avulsion injury: Medial pectoral nerve may be transferred to the musculocutaneous nerve or the biceps branch or a fascicle from the ulnar nerve (Oberlin transfer) can be transferred to the motor branch of the biceps.
- Secondary reconstructive options: tendon/ muscle transfer, free muscle transfer, arthrodesis, osteotomy
- Shoulder Arthrodesis: consider for patients with severe restricted shoulder passive ROM, significant bone loss or failed prior reconstructive measures.
Brachial Plexus Surgical Considerations
- Consider intraoperative electrodiagnostic studies. Nerve action potentials (NAPs) and somatosensory evoked potentials (SSEPs), as well as CMAPs. NAPs allow testing directly across a lesion to detect reinnervation months before conventional EMG. The presence of a NAP across a lesion indicates preserved axons or significant regeneration; recovery will occur after neurolysis alone. SSEP's indicate continuity between the peripheral nervous system and the central nervous system via a dorsal root. SSEPs are absent in postganglionic or combined pre- and postganglionic lesions.
Brachial Plexus Associated Injuries / Differential Diagnosis
Brachial Plexus Complications
- Contractures
- Pain syndromes
- Loss of function
Brachial Plexus Follow-up Care
- Dependent on treatment chosen. All patients require extensive physical therapy.
Brachial Plexus Review References
- Rühmann O, Gossé F, Wirth CJ, Schmolke S: Reconstructive operations for the paralyzed shoulder in brachial plexus palsy: Concept of treatment. Injury 1999;30:609-618.
- Shin AY, JAAOS, 2005;13:382
|