|
|
synonyms: Tommy John procedure, Elbow UCL reconstruction, ulnar collateral ligament (UCL) reconstruction; valgus elbow instability; overhead athlete; Tommy John surgery
MCL Reconstruction CPT
MCL Reconstruction Indications
- Elbow MCL instability in elite athletes.
- Elbow MCL instability which has failed non-operative management. Minimum, 6 weeks of throwing abstinence followed by rehabilitation to address pitching mechanics and shoulder motion deficits and core strengthening.
MCL Reconstruction Contraindications
MCL Reconstruction Alternatives
- Direct MCL repair (indicated only for patients with acute avulsion injuries)
- Non-operatitve treatment
MCL Reconstruction Pre-op Planning / Special Considerations
- Graft options: palmaris longus, 4th toe extensor tendon, plantaris tendon, gracilis tendon.
- Reconstruction Techniques: Modified-Jobe Technique (Thompson WH, JSES 2001;10:152), modified-Docking Technique (Paletta GA Jr AJSM 2006;34:1594), Interference Screw technique (Conway JE, Tech Shoulder Elbow Surg 2006;7:36). New TOFU technique has been shown to be biomechanically superior (Shah RP, JSES 2009;18:58).
- Ulnar nerve transposition is associated with increased risk of ulnar neuropathy (Vitale MA, AJSM 2008;36:1193).
- Modified docking techique has been shown to have improved outcomes to Jobe technique (Vitale MA, AJSM 2008;36:1193).
MCL Reconstruction Technique
- Sign operative site in pre-op area
- Pre-operative antibiotics, +/- regional block
- Supine on the operating table. All bony prominences well padded.
- General anesthesia
- examination of the elbow under anesthesia
- Prep and drape in standard sterile fashion.
- limb is exsanguinated, tourniquet inflated to 250 mm Hg.
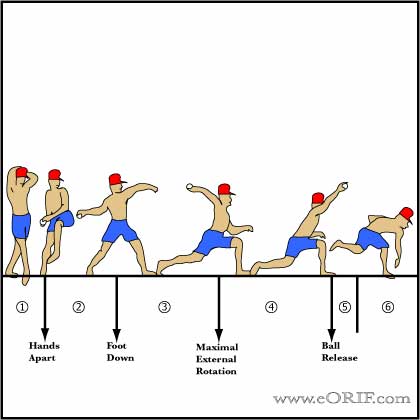
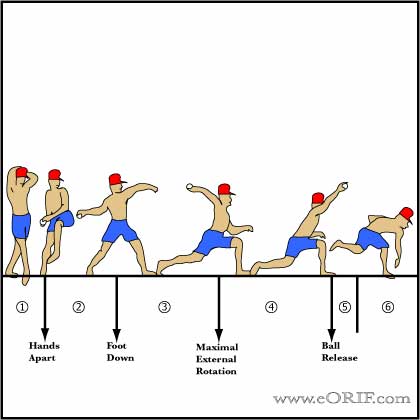
- anterolateral arthroscopic portal: evaluate anterior compartment articular surfaces and synovium; perform arthroscopic valgus stress test at 70° of flexion with the arm pronated (medial opening > 1mm suggests UCL insufficiency
- medial incision centered over the medial epicondyle
- Identify and protect the medial antebrachial cutaneous nerve with a vessel loop
- Dissect out the ulnar nerve from the cubital tunnel and protected with a vessel loop.
- continue release proximally to the arcade of Struthers and distally into the flexor carpi ulnaris muscle mass.
- Remove a portion of the medial intermuscular septum to prevent tenting of the ulnar nerve
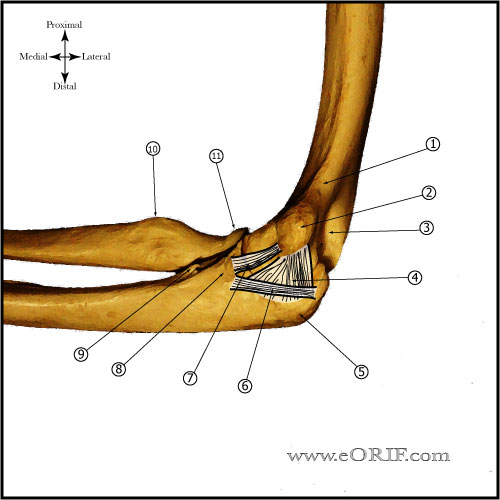
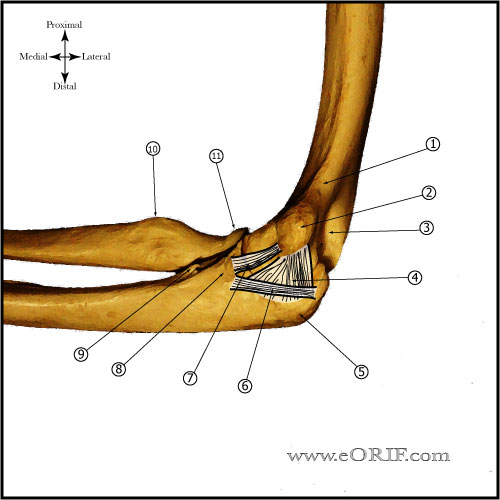
- Expose the anterior band by elevation of the flexor muscles from the UCL distal sublime tubercle attachment.
- Inspect the ligament for attenuation or tearing
- Incise the ligmanet longitudinally and visualization the deep portion
- If concomitant valgus extension overload with olecranon osteophytes is suspected, perform a vertical posterior capsulotomy proximal to the fibers of the posterior band of the UCL exposing the olecranon tip and remove any osteophytes with a small osteotome and high-speed bur.
- Probe the posterior compartment for loose bodies or articular cartilage damage / kissing lesion of the trochlea.
- Close the capsulotomy with absorbable suture.
- Graft harves: Ipsilateral Palmaris longus tendon / gracilis / plantaris / toe extensor tendon.
- Palmaris longus harvest: 3 small incisions on the volar forearm, beginning at the proximal wrist crease. Assure harvest of the palmaris longus tendon rather than FCR tendon. Ensure median nerve which lies deep to the palmaris longus tendon is protected
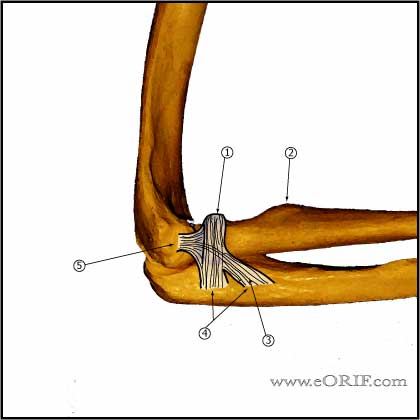
- Drill Tunnels with a 3.2-mm drill bit in the ulna and medial epicondyle
- Single ulnar tunnel is made by placing two ulnar 3.2mm drill holes at the native attahment 3 to 4 mm distal to the articular surface of the coronoid process, separated by 1 cm.
- Two medial epicondylar tunnels are placed along the proximal portion of the epicondyl and converge at the origin of the native ulnar collateral ligament.
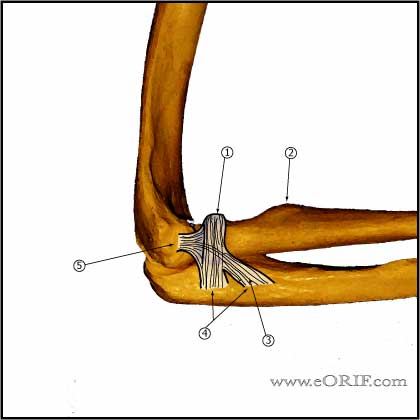
- Repair the native ligament remnant with nonabsorbable suture
- Passed the graft in a figure-eight fashion.
- Apply varus stress with the elbow at 30° of flexion and secured the graft side-to-side with multiple nonabsorbable sutures.
- Transpose the ulnar subcutaneously and secure with a loosely tensionted single fascial sling from the flexorpronator muscle fascia.
- Irrigate
- Close in layers
- Splint elbow at 90° of flexion
MCL Reconstruction Complications
- Ulnar nerve palsy / transient ulnar nerve neuropraxia: most common complication.
- Cubital tunnel syndrome / Ulnar Neuritis
- Flexor-Pronator mass avulsion / morbidity
MCL Reconstruction Follow-up care
MCL Reconstruction Outcomes
- 93% excellent results with modified Jobe technique in highly competitive athletes who had not had a prior surgical. All athletes, regardless of whether they had a prior procedure, were able to return to their sport. (Thompson WH, JSES 2001;10:152).
- 90% return to sport with docking technique (Dodson CC, AJSM 2006;34:1926).
- 83% exellent result. 10% complication rate (6% ulnar neuropathy). Better outcome with muscle splitting approach. Better results without ulnar nerve transposition. Best results with modified docking technique (Vitale MA, AJSM 2008;36:1193)
MCL Reconstruction Review References
- Conway JE, Oper Tech Sports Med 2001;9:196
- Thompson WH, JSES 2001;10:152
- Williams RJ III, ICL 2004;53:579
- Bruce JR, Andrews JR. Ulnar collateral ligament injuries in the throwing athlete. J Am Acad Orthop Surg. 2014 May;22(5):315-25. doi:10.5435/JAAOS-22-05-315
- Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008 Jun;36(6):1193-205.
- Operative Elbow Surgery: Expert Consult: 2012

- AAOS/ASES Advanced Reconstruction Elbow, 2007

- Orthopaedic Knowledge Update: Shoulder and Elbow, No. 3
- Cain EL Jr, Andrews JR, Dugas JR, Wilk KE, McMichael CS, Walter JC 2nd, Riley RS, Arthur ST. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: Results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010 Dec;38(12):2426-34.
|