|






|
synonyms: tibia fracture, tibial shaft fracture
Tibial Shaft Fracture ICD-10
Tibial Shaft Fracture ICD-9
- 823.22 (closed, shaft of tibia and fibula)
- 823.32 (open, shaft of tibia and fibula)
Tibial Shaft Fracture CPT
Tibial Shaft Fracture Etiology / Epidemiology / Natural History
- Most common long bone fx
- @time to union=19-21wks, 20wks for stable, low-energy, >30wks unstable, high-energy
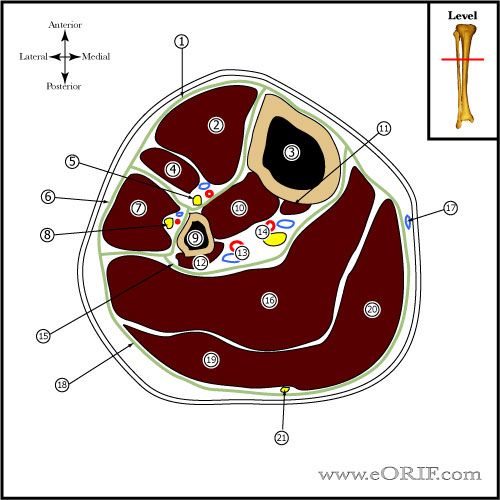
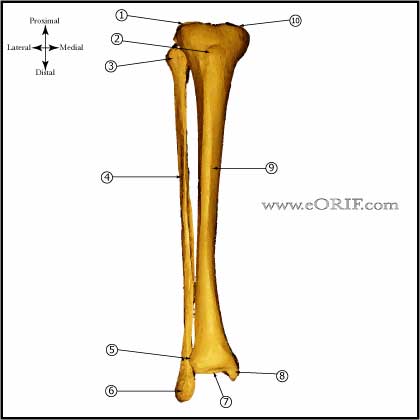
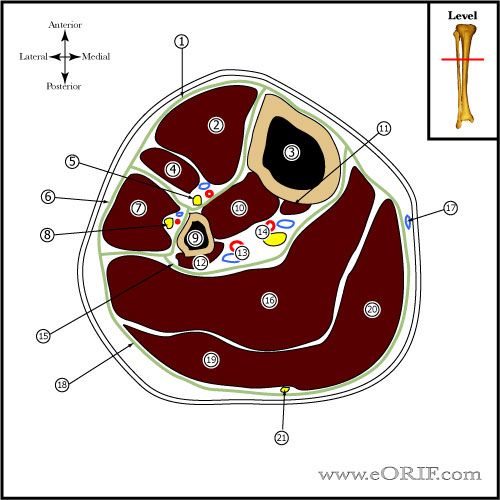
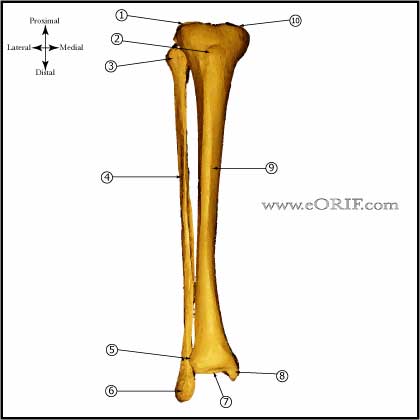
Tibial Shaft Fracture Anatomy
- Size ranges from 30-47cm in adults, intramedullary diameter =8-15mm
- Proximal tibia has average 15 degree apex anterior angulation
- Radius of supramalleolar curvature is approximately 20cm, ie medial surface turns medially @25degrees.
- Diaphyseal blood supply is via a single nutrient artery, the proximal branch of the posterior tibial artery which passes through the most proximal portion of the tibialis posterior to obliquely enter the tibial shaft on its posterior surface in the proximal portion of the middle third of the bone. Only peripheral 1/3-1/4 of diaphyseal cortex is supplied by periosteal vessels.
- Fibula bears 6-17% of body weight, fibular head is attachment for LCL and biceps femoris, common peroneal nerve wraps around fibular neck.
- Interosseous membrane fibers run downward and laterally
Tibial Shaft Fracture Clinical Evaluation
- Leg pain, inability to bear weight, contusions, deformity
- Evaluate extent of soft tissues, open fracture injury
- Document neurovascular exam before and after any treatment
- Evaluate for Compartment Syndrome.
Tibial Shaft Fracture Xray / Diagnostic Tests
- A/P and Lateral, must include ankle and knee
- get CT if near ankle or knee
Tibial Shaft Fracture Classification / Treatment
- Generally descriptive(proximal, middle, distal, transverse, oblique, spiral, segemental, comminuted)
- Treatment Options = casting (negligible infection, no knee pain, no HWR) , Ex Fix(no disruption of soft tissue envelope), ORIF, IM nail(better alignment, early ROM, improved mobility, less frequent f/u, earlier return to work)-treatment remains controversial
- Low energy, stable pattern(spiral): <1cm shortening, <5° angulation, <5° rotation, competent soft tissues
-Treatment = Long leg cast
-Intact fibula has 25% incidence of varus malunion with cast treatment. Teitz CC,JBJS 1980 Jul;62A(5):770-6
- High Energy, unstable pattern:>1cm shortening, >5° angulation, >5° rotation, incompetent soft tissues
-Treatment = IM nail.
- Severe soft tissue injury, unstable patient:
-Treatment = External Fixation. Type IIIB injuries are better treated with IM nailing than external fixation (Dervin GF, CORR 1996;332:10), (Schandelmaier P, CORR 1997;342:164).
- Proximal 1/3 Shaft fracture: Strong tendency for valgus and flexion deformity.
-Treatment: IM Nail vs Locked submuscular plating.
- AO Classification, (AO/OTA J Orthop Trauma 1996;10 Suppl 1:v-ix, 1/154)
Tibial Shaft Fracture Associated Injuries / Differential Diagnosis
Tibial Shaft Fracture Complications
- Delayed union
- Nonuion2-5%
- Infection: 1-3%
- NVI
- Contracture
- Malunion / angular deformity: 2-5%
- Compartment Syndrome: 2-5%
- Late loss of alignment (External fixation) delayed union,
- Pin infection (External fixation)
- Knee pain=40-56% (Court-Brown CM, JOT 1997;11:103), (Keating JF, JOT 1997;11:10).
- DVT / PE
- CRPS
Tibial Shaft Fracture Follow up care
- If minimal callus is formed at 6-8wks after IM nailing, nail dynamization is indicated
- very common to have anterior knee pain s/p IM nail, 90% resolves after nail removal. Must wait till 18months to remove nail
Amputation vs Salvage
- dismal results for salvaged IIIc fxs-Caudle, JBJS 69:801 1987
- longer more severe disability, more complications, poorer outcomes comparing IIIB to salvage. Georgiadis, JBJS 75A:14431, 1993
- increased morbidity, mortality, extreme costs, delayed recovery with delayed amputation. Bondurant J trauma 28:1270 1988: Clarke, Injury 25:139 1994: Pozo JBJS 72B:288 1990
- 15 pts with infected nonunions and delayed amputations averaged 12 operations, 8 months hospitalization and >50 months before amputation. 6 months rehabilitation before employment after BKA. Pozo JBJS 72B:288 1990
- Court-Brown, et. al. (JBJS 77-B, No. 3, May 1994) reviewed 33 cases of uninfected non-union of the tibia. Exchange nailing was successful in closed fractures, and open fractures of Gustilo types I, II, and III A. Exchange nailing failed in those fractures with bone loss of more than 2 cm and 50% of the circumference. For these fractures the authors recommend the early use of bone grafting.
- Georgiadis GM, Behrens FF, Joyce MJ, et al: Open tibial fractures with severe soft-tissue loss: Limb salvage compared with below-the-knee amputation. J Bone Joint Surg 1993;75A:1431-1441.
- Drischl DR, Dahners LE: The mangled extremity: When should it be amputated? J Am Acad Orthop Surg 1996;4:182-190.
- Hansen ST Jr: Overview of the severely traumatized lower limb: Reconstruction versus amputation. Clin Orthop 1989;243:17-19.
Tibial Shaft Fracture Referneces
- Rockwood and Green's Fractures in Adults: 2009
- Watson JT, Treatment of Unstable fractures of the shaft of the Tibia, JBJS 76A:1575-1584, 1994
- Hooper GJ, JBJS 73B:83-85, 1991
- Sarmiento A. et al. Factors influencing the outcome of closed tibial fractures treated with functional bracing. Clin. Orthop. 1995; 315:pp. 8-24.
- Singer RW, Kellam JF: Open tibial diaphyseal fractures: Results of unreamed locked intramedullary nailing. Clin Orthop 1995;315:114-118.
- Bone LB, Kassman S, Stegemann P, et al: Prospective study of union rate of open tibial fractures treated with locked, unreamed intramedullary nails. J Orthop Trauma 1994;8:45-49.
- °
|