|
|
synonyms: shoulder instability, anterior dislocation, shoulder dislocation, shoulder subluxation
Shoulder Dislocation ICD-10
A- initial encounter
D- subsequent encounter
S- sequela
Shoulder Dislocation ICD-9
- 831.01(anterior)
- 831.02(posterior)
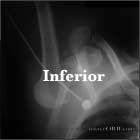
- 831.03(inferior)
- 718.81 (instability of shoulder joint)
Shoulder Dislocation Etiology / Epidemiology / Natural History
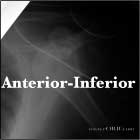
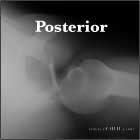
- >90% are anterior dislocations. <3% posterior dislocations.
- 85% associated with Bankart Lesion
- Anterior dislocations generally result from forced external rotation or extension in an abducted and externally rotated arm.
- Posterior dislocations: associated with epileptic seizures, high-energy trauma, electrocution, or electroconvulsive therapy. Seizures may be associated with hypoglycemia(diabetes) or drug withdrawl
- Incidence = 1.69/1000 person years in US military; 0.08/1000 person years in general US population (Owens BD, JBJS 2009;91A:791).
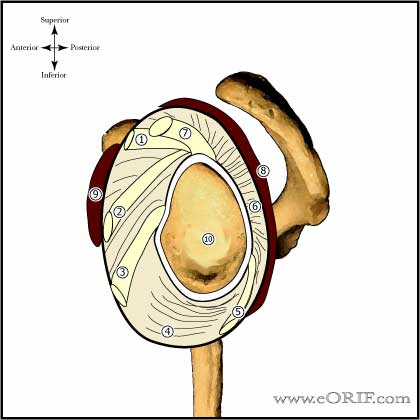
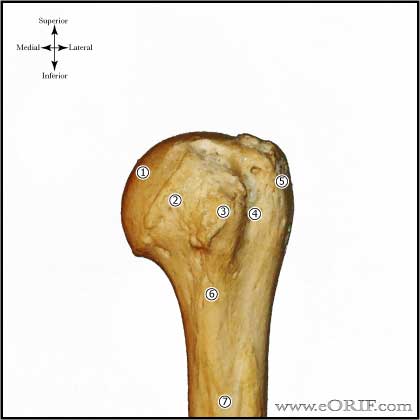
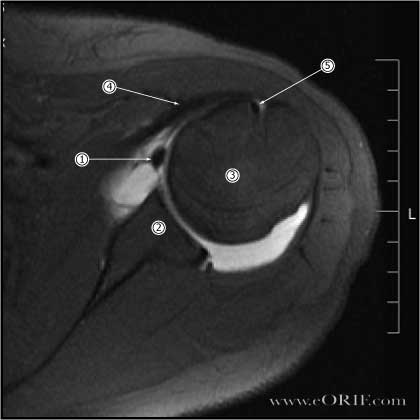
Shoulder Dislocation Anatomy
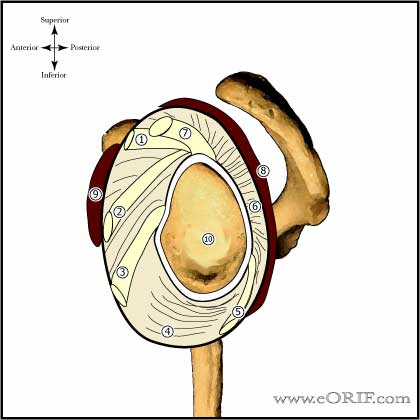
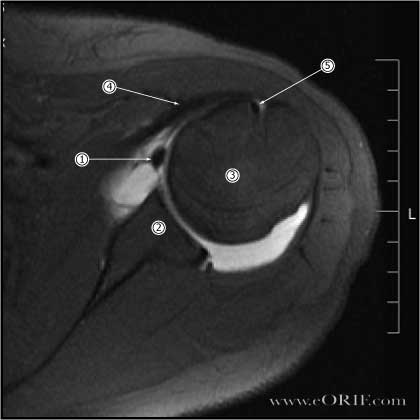
- Glenohumeral stability is dependent on static (labrum, GH capular ligmants) and dynamic (RTC, deltoid, biceps, scapular musculature) restraints.
- Inferior glenohumeral ligament(consist of anterior inferior GH ligamant, axillary pouch and posterior inferior GH ligament) is the most important for resisting anterior translation in the abducted arm.
- See also Shoulder Anatomy.
Shoulder Dislocation Clinical Evaluation
- Anterior dislocations: prominence of the humeral head anterior, medial and inferior to the shoulder joint with a hollow region beneath the lateral deltoid. Loss of normal deltoid contour with prominent anterior acromion. Arm is held in an abducted, sligthly externally rotated position.
- Posterior dislocations: prominence of humeral head posteriorly with prominent coracoid process anteriorly. Arm is held in an internally rotated, adducted position. Inability to externally rotate arm.
- Inferior dislocation: arm is generally locked in an overhead position; horizontally abducted.
- Evaluate for Axillary Nerve function. Humeral head may compress the axillary nerve.
- Complete UE neurovascular exam, include brachial, radial and ulnar pulses.
Shoulder Dislocation Xray / Diagnositc Tests
- A/P, and Lateral in the plane of the scapula, and Axillary view. Closely evaluate for concomitant surgical neck or other fracture.
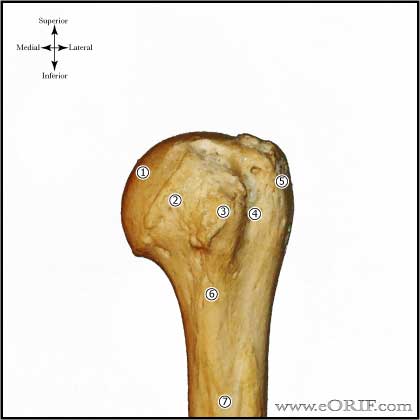
- Hill-Sachs lesion is an impression fracture of the posterosuperior aspect of the humeral head, produced by contact with the anteroinferior glenoid when dislocated. Hill-Sachs lesion is demonstrated on plain AP radiograph in internal rotation.
- MRI indicated to evaluate for Bankart Lesionin young athletic patients and RTC tears in older patients.
- CT scan is best to evaluate bony anatomy and should be considered for the recurrent dislocator suspected of having a large Hill-Sachs or bony Bankart lesion.
Shoulder Dislocation Classification / Treatment
- Anterior: closed reduction, document neurovascular status before and after reduction; multiple reduction techniques reported. If seen immediately after injury, one attempt at closed reduction before Pectoralis major spasm sets in is indicated, even without xrays . Once spasm sets in pain medications are often needed before attempting reduction. Consider immobilzation in adduction and external rotation. Consider primary Anterior-Inferior Glenohumeral Instability Repair for highly athletic young (<25y/o) patients with MRI confirmed Bankart Lesion, (Handoll HH, Cochrane 2004;1:CD004325), (Jakobsen BW, Arthroscopy 2007;23:118). Patients >40y/o should be treated with a sling for comfort with mobilization as tolerated +/- physical therapy to strengthen the dynamic stabilizers about the shoulder, consider RTC repair for those patients with MRI documented tears. Immobilization in 30 of external rotation has shown a decreased recurrence rate. (Itoi E, JSES 2003;12:413), (Itoi E, JBJS 2001;83A:661).
- Non-operative treatment in young patients: Immobilization for 3-5 weeks followd by strengthening exercises and the avoidance of abduction. Restrict activity level / sports for at least 6 weeks. 75% success rate, 25% failure rate. (Aronen JG, AJSM, 1984;12:283). 92% failure rate (Wheeler JH, Arthroscopy 1989;5:213).
- Nonoperative treatment for first time dislocation in-season athlete: average return to play 10.2 days. 37% recurrent dislocation in season. (Buss, DA, AJSM 2004)
- First Time dislocation in young males: 65-92% recurrent instablility for non operative treatment. 14% recurrent instability with arthroscopic Bankart repair.
- Acute Posterior: reduction is performed with lateral traction, external rotation and abduction; considering applying slight forward flexion, internal rotation and adduction initially to dislodge humeral head. Document neurovascular status before and after reduction.Immobilize in slight extension and external rotation followed by physical therapy. Redislocation is likely if reverse Hill-Sachs lesion is >20% of humeral head.
- Inferior: ensure mechanism is consistant with inferior dislocation. Axillary nerve palsy, deltoid atony or other shoulder trauma may cause inferior GH subluxation which will resolve with simple observation. If injury is a traumatic disolcation treatment = closed reduction, document neurovascular status before and after reduction. See also Luxatio Erecta.
- Chronic Posterior Dislocation: closed reduction is ineffective after 4-6 weeks. Open reduction with lesser tuberosity /subscap transfer indicated for defects of 20-45%. Hemiarthroplasty indicated for defects of 50-60%. Consider total shoulder for elderly patients with arthritis.
- Chronic Anterior Dislocation: generally associated with humeral head and glenoid bone loss which prevents maintenance of reduction: TSA vs hemiarthroplasty. (Matsoukis J, JBJS 2006;88A;547).
- Burkhead and Rockwood Classification- traumatic/atraumatic subluxation
Type I =traumatic subluxation without previous dislocation
Type II =traumatic subluxation after previous dislocation
Type IIIA =atraumatic, voluntary subluxation in patients with psychological problems
Type IIIB =atraumatic, voluntary subluxation in a patient without psychological problems
Type IV =involuntary subluxation.
They found traumatic instability (type I or type II) = 15% good or excellent outcome with a rehab program. Atraumatic subluxations (type III or type IV) = 83% good to excellent result.
Shoulder Dislocation Associated Injuries / Differential Diagnosis
Shoulder Dislocation Complications
- Recurrent instability:
-Nonop treatment: higher incidence of instability in younger patients with acute traumatic dislocations; 90% in athletic patients <20y/o; 15% in patients >40 y/o; glenoid rim fractures. Consider shoulder arthrodesis in patients with painful shoulders who have failed multiple previous reconstructive attempts.
-Postoperative recurrence: related to attritional glenoid bone loss, large Hill-Sachs defect, inferior and/or anterior hyperlaxity, use of 3 or fewer suture anchors. (Boileau P, JBJS 2006;88A:1755)
- Axillary Nerve Palsy
- Brachial Plexus Palsy
- Axillary artery injury
- Osteonecrosis: rare; generally associated with fracture-dislocations. Best treated with observation in adolescents (Pateder DB, JBJS 2004;86A:2290).
Shoulder Dislocation Follow-up Care
- After reduction patients are generally immobilized for 4-6 weeks in a sling. Consider immobilzation in adduction and external rotation. Immobilization in 30 of external rotation has shown a decreased recurrence rate. (Itoi E, JSES 2003;12:413), (Itoi E, JBJS 2001;83A:661).
- Non-op outcomes: 87% return to sport, average time out of sport = 10.2 days. 53% later require surgery. (Buss DB, AJSM 2004;32:1430).
- In-Season Athletes: 87% able to return to sport in same season, average 10 days post injury; 33% recurrence; 54% eventually require surgery. (Lynch GP, AJSM 2004;32:1430).
- 9% of non-surgically treated patients develop osteoarthritis at 10 years (Hovelius L, JBJS 1996;78A:1677).
- 14% moderate to severe OA when treated with Bristow-Laterjet procedure (coracoid transfer) (Hovelius L, JSES 2006;15:279).
- Shoulder Outcome measures
Shoulder Dislocation Review References
- Lee D, Operative Techniques: Shoulder and Elbow Surgery: Book, Website and DVD, 1e, 2010

- Craig EV, The Shoulder (Master Techniques in Orthopaedic Surgery), 2012
- Williams GR, Operative Techniques in Shoulder and Elbow Surgery, 2010
- Sonnabend DH: Treatment of primary anterior shoulder dislocation in patients older than 40 years of age: Conservative versus operative. Clin Orthop 1994;304:74-77.
- Gumina S, Postacchini F: Anterior dislocation of the shoulder in elderly patients. J Bone Joint Surg 1997;79B:540-543.
- Hovelius L, JBJS 1996;78A:1677.
|