|


|
synonyms:tibial plateau fracture ORIF, proximal tibial fracture ORIF
ORIF Tibial Plateau CPT
ORIF Tibial Plateau Indications
- Open Fracture
- Compartment Syndrome
- Vascular injury
- Displaced bicondylar fx
- Displaced medial condyle fx
- Lateral plateau fx with joint instability
- Articular depression(>2mm)
- >10 degrees varus/valgus instability
ORIF Tibial Plateau Contraindications
- Soft Tissue Injury: Open treatment is applicable if: (1)absence of fx blisters, (2)able to palpate all bony landmarks, (3)absence of extensive subq hemorrhage, (presence of skin wrinkles)
ORIF Tibial Plateau Alternatives
- External Fixation
- Ilizarov
ORIF Tibial Plateau Pre-op Planning / Special Considerations
- Pre-operative plan surgery based on Xrays/CT (consider xrays of normal leg / traction views) using AO technique.
- Equipement: proximal tibial plates, femoral distractor, osteotomes, suture anchors, knee athrsocopy equipement, bone tamps, bone graft substitute radiolucent OR Table.
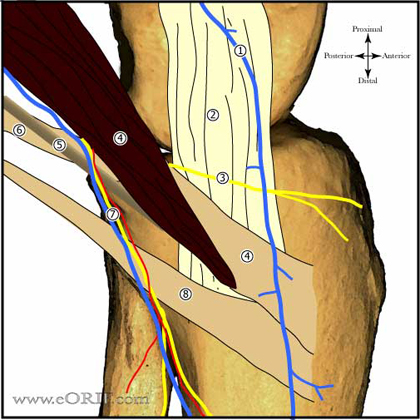
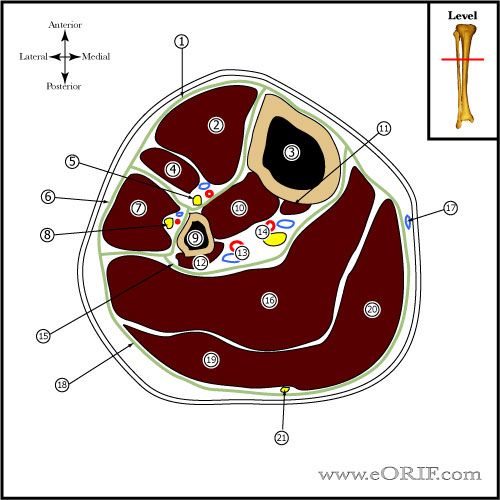
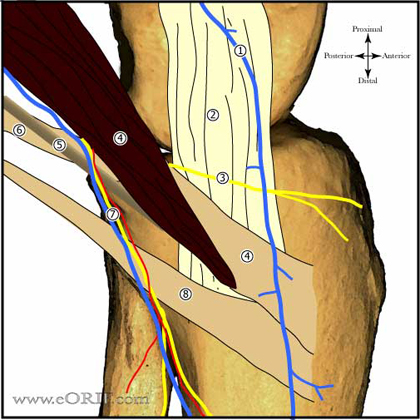
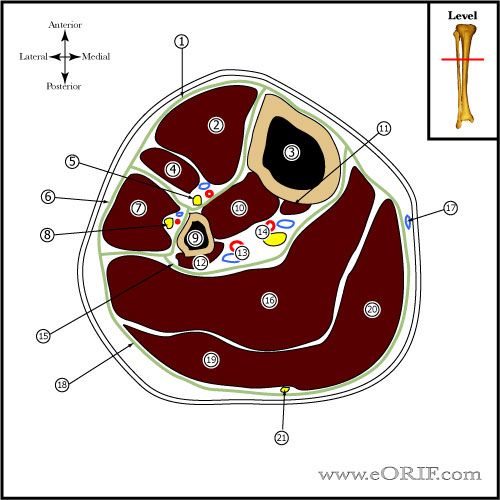
- Approach / incision is dependent on fracture location, soft tissue injury and fixation needs. Lateral plateau = lazy "S" or "L" incision. Medial plateau fractures = medial parapaellar or posteromedial approach. Bicondylar = lateral "L" incision with posteromedial approach.
- Goals=anatomic joint line and restored mechanical LE alignment
- Consider calcium phosphate cement augmentation of depressed segment (Trenholm A, JOT 2005;19:698).s
ORIF Tibial Plateau Technique
- Pre-op antibiotics, supine, C-arm placed on opposite side of table.
- EUA of knee, Perform varus/valgus stress testing with the knee near full extension under fluoro. Any opening >10 degrees indicates collateral ligament injury.
- Place well padded tourniquet high on the thigh. Consider placing leg in knee holder with ankle distractor for ligamentotaxis reduction or use femoral distractor or external fixation for ligamentotaxis reduction. Verify A/P, lateral and oblique fluroscopic images can be taken.
- Prep and drape R/L lower extremity in standard sterile fashion. Drape out iliac crest if needed.
- Leg exsanginated with Eschmar bandage and tourniquet inflated
- Perform limited Knee Arthroscopy evacuating hematoma, evaluate articular surface and for associated injury. Arthroscopy is generally not useful for Type IV-VI fractures due to loss of capsular integrity / extravasation.
- Perform anterior compartment fasciotomy with Metzenbalm scissors.
- 2-pin ex fx vs femoral distraction vs non-invasive ankle distractor to achieve ligamentotaxis reduction; percutaneous reduction clamp assistance as needed.
- Reduction is held with k-wires which may be exchanged for 6.5mm or 7.3mm cannulated screws.
- Joint reduction can be confirmed fluroscopically(less dissection) vs submeniscal exposure(increased dissection), arthroscopically(risk compartment syndrome / extravasation). Verify anatomic reduction, length, rotation, varus, valgus and recurvatum.
- Generally laterally based plate via lateral peripatellar approach.
- LISS Plate (Synthes)-Assemble guide to plate. Insert plate between anterior tibialis and periosteum; Place 2.0mm k-wires into proximal k-wire holes (or fixation points) parallel to joint; place distal hole 2.0mm k-wire; verify plate alignment in a/p and lat planes, Minimum of 4 5.0mm titanium locking screws in each fragment are recommended. Ensure that proximal posterior screw does not exit cortex. Cortical screws are best inserted with high-speed, limited pressure. Final tightening by hand. Always place screw in hole A(proximal second row single hole) last.
- Consider medial buttress semitubular plate usually via small posteromedial incision for Type IV-VI fractures. If soft tissue injury prohibits medial exposure use monolateral ex fx (Christensen, JOT 4:226, 1990)
- Elevate any depressed fragments using bone tamps through fracture line, or by making a cortical window and fill any void with auto/allo bone graft or bone graft substitute.
- Irrigate.
- Incision closed in layers
- Post-operatively patient is placed in hinged knee brace, 30 lbs weight-bearing for 8-12 wks.
ORIF Tibial Plateau Complications
- Stiffness
- Infection(up to 12%)
- Malunion
- Nonuion
- Loss of fixation
- Skin loss
- Amputation
- Extensile exposures in tenous soft tissue can lead to complication rates as high as 50%
- Post-traumatic arthritis
- Painful hardware
- Peroneal nerve palsy
- DVT/PE
- Compartment Syndrome
- CRPS
- Heterotopic Ossification
- The risks of surgery include but are not limited to: Incomplete releif of pain incomplete return of funtion, Stiffness, Infection, Malunion, Nonuion, Loss of fixation, Skin loss, need for amputation, Post-traumatic arthritis, Painful hardware, nerve or vascular injury, DVT/PE, Compartment Syndrome, CRPS, DVT / PE, Heterotopic Ossification and the risks of anetsthesia including heart attack, stroke and death.
ORIF Tibial Plateau Follow-up care
- Post-op:
- 7-10 Days:
- 6 Weeks:
- 3 Months:
- 6 Months:
- 1Yr:
ORIF Tibial Plateau Outcomes
- (Stannard JP, JOT 2004;18:552).
- (Weigel DP, JBJS 2002 84A;1541).
ORIF Tibial Plateau Review References
- Watson JT, Wiss DA, in Masters Techniques, Fractures, 2005
- Rockwood and Green's Fractures in Adults: 2009
|